Microfiltración marginal en incrustaciones de cerómero tipo table top cementadas con cementos resinosos: autograbantes, universales y resina termoplastificada
Wear of the enamel by different chemical and mechanical treatments
Desgaste do esmalte por diferentes tratamentos químicos e mecânicos
Jennifer Gabriela Risco Tigua1, Eddy Jhonny Álvarez Lalvay2
RECIBIDO: 18/12/2018 ACEPTADO: 29/03/2019 PUBLICADO: 01/12/2019
- Estudiante de la Facultad de Odontología; Universidad Central del Ecuador; Quito, Ecuador.
- Docente de la Facultad de Odontología; Universidad Central del Ecuador; Quito, Ecuador.
CORRESPONDENCIA
Eddy Jhonny Álvarez Lalvay
Universidad Central del Ecuador;
Facultad de Odontología
ejalvarez@uce.edu.ec
RESUMEN
Luego del procedimiento de cementación de incrustaciones de cerómero puede presentarse microfiltración en la interfase diente-restauración, el gap en la interfase puede ser influenciado por las características del agente cementante y el proceso de cementación. Objetivo: Evaluar la microfiltración en incrustaciones de cerómero tipo table top cementadas con tres diferentes cementos. Materiales y métodos: En 36 terceros molares divididos en 3 grupos (n= 12), se realizaron preparaciones estandarizadas tipo table top y se fabricaron incrustaciones con CERAMAGE® (SHOFU, Japón) que fueron cementadas con 3 biomateriales diferentes, Grupo A: cemento de autograbado RelyX® U200 (3M). Grupo B: cemento universal RelyX Ultimate® (3M, USA). Grupo C: resina termo plastificada a 55oC Enamel Plus HRI® (Micerium). Cada muestra se sometió a termociclado (3300 ciclos) y se colocaron en una solución de azul de metileno durante 24 horas. Para el análisis se realizó un corte longitudinal en la zona media en sentido meso-distal de las muestras y se evaluó la microfiltración marginal en la cara mesial y distal con la ayuda de un estéreo microscopio Olympus. Los resultados se almacenaron en una base de datos en Excel, posteriormente los valores experimentales se archivaron y fueron codificados utilizando el software BioEstat (Brasil). El análisis se realizó mediante la prueba no paramétrica de Kruskal Wallis, con una significancia del 95%. Resultados: La resina termo plastificada presentó los valores más bajos en el grado de microfiltración con una media de 0,4mm; con el cemento universal se obtuvo los valores más altos con una media de 1,33 mm, que no fue significativa en relación al cemento de autograbado que tuvo una media de 0,88 mm. Conclusiones: Se logró determinar que en restauraciones tipo table top el grado de microfiltración fue menor cuando se cementaron con resina termo plastificada (p= <0,05) con una diferencia estadísticamente significativa respecto a los otros cementos. No existió diferencia en la microfiltración entre los cementos de resina de autograbado en relación al cemento de resina universal.
Palabras clave: Esmalte dental; pulido dental / métodos; esmalte dental / efectos farmacológicos; microabrasión / métodos de esmalte; abrasión de aire.
ABSTRACT
After the process of cementation of cerometer encrustations, microfiltration can occur in the tooth-restoration interface, the gap in the interface can be influenced by the characteristics of the cementing agent and the cementation process. Objective: To evaluate the microfiltration in inlays of ceramics type table top cemented with three different cements. Materials and methods: In 36 third molars divided into 3 groups (n = 12), standardized table top preparations were made and inlays made with CERAMAGE® (SHOFU, Japan) that were cemented with 3 different biomaterials, Group A: cement RelyX® U200 self-etch (3M). Group B: RelyX Ultimate® universal cement (3M, USA). Group C: thermoplastic resin at 55oC. Each sample was subjected to thermocycling (3300 cycles) and placed in a solution of methylene blue for 24 hours. For the analysis, a longitudinal cutting was made in the middle area in the meso-distal direction of the samples and the marginal microfiltration on the mesial and distal side was evaluated with the help of an Olympus stereo microscope. The results were stored in a database in Excel, then the experimental values were archived and coded using the BioEstat software (Brazil). The analysis was performed using the non-parametric Kruskal Wallis test, with a significance of 95%. Results: The thermoplastic resin had the lowest values in the degree of microfiltration with an average of 0.4mm; with the universal cement the highest values were obtained with an average of 1.33mm, which was not significant in relation to the self-etched cement that had an average of 0.88mm. Conclusions: It was possible to determine that in table type restorations the degree of microfiltration was lower when they were cemented with thermoplasticized resin (p = <0.05) with a statistically significant difference with respect to the other cements. There was no difference in microfiltration between self-etched resin cements in relation to universal resin cement.
Keywords: Dental inlays; marginal adaptation; dental filtration; resin cements; cementation.
RESUMO
Após o processo de cimentação das incrustações de cerômero, pode ocorrer microfiltração na interface dente-restauração, o espaço na interface pode ser influenciado pelas características do agente cimentante e do processo de cimentação. Objetivo: Avaliar a microfiltração em incrustações tipo “table top” de cerómero cimentada com três cimentos diferentes. Materiais e métodos: Em 36 terceiros molares divididos em 3 grupos (n = 12), foram preparadas restaurações padronizadas tipo “table top”, após, incrustações foram confeccionadas com CERAMAGE® (SHOFU, Japão) e cimentadas com 3 biomateriais diferentes, Grupo A: cimento Autocondicionante RelyX® U200 (3M). Grupo B: cimento universal RelyX Ultimate® (3M, EUA). Grupo C: Resina termoplástificada Enamel Plus HRI® 55°C (Micerium). Cada espécime foi submetido a termociclagem (3300 ciclos) e colocado em uma solução de azul de metileno por 24 horas. Para a análise, foi feita uma seção longitudinal na área do meio na direção meso-distal das amostras e avaliada a microfiltração marginal em mesial e distal com a ajuda de um estéreo microscópio Olympus. Os resultados foram armazenados em um banco de dados em Excel, e os valores experimentais foram arquivados e codificados no software BioEstat (Brasil). A análise foi realizada pelo teste não paramétrico de Kruskal Wallis, com significância de 95%. Resultados: A resina termoplástificada apresentou os menores valores no grau de microfiltração com média de 0,4mm; com o cimento universal, os valores mais altos foram obtidos com média de 1,33mm, o que não foi significativo em relação ao cimento autocondicionado, com média de 0,88mm. Conclusões: Foi possível determinar que nas restaurações tipo “table top” o grau de microfiltração foi menor quando cimentadas com resina termoplástica (p = <0,05), com diferença estatisticamente significante em relação aos demais cimentos. Não houve diferença na microfiltração entre os cimentos resinosos autocondicionantes em relação ao cimento resinoso universal.
Palavras-chave: Incrustações; adaptação marginal; infiltração dentária; cimentos resinosos; cimentação.
INTRODUCTION
The indirect restoration technique refers to the manufacture of the restoration outside the oral cavity in the laboratory, after which it is placed on the tooth some cementing agent; in addition, it allows conventional photopolymerization, the use of heat (140°C), pressure (0.6 MPa for 10 min) and nitrogen atmosphere; improving the physical properties, in addition a greater degree of polymerization is achieved and the polymerization contraction does not occur in the prepared tooth, so the strain is reduced1.
However, there are complications; In this sense, microfiltration is of major relevance because it can determine the failure of the procedure due to improper sealing, they are responsible for postoperative sensitivity, degradation of the hybrid layer, marginal staining, infiltration of bacteria and oral fluid, which can lead to secondary caries. Microfiltration is a dynamic phenomenon that allows bacteria, fluids, molecules and ions to pass through the interface of the restoration and the walls of the cavity; however, in some cases, it is not clinically obvious.
There are several types of resin to cement an indirect restoration; they differ in the treatment of the tooth surface before the application of cement. Authors such as Bucheli & Mena, 20172, recommend the use of thermo-plasticized resins as cementing agents in indirect restorations; However, self-adhesive cements have attracted interest because they do not require any prior treatment of the dentin surface and are easy to use.
It has been stated that the samples that have the lowest marginal microfiltration are those cemented with preheated resin2. however, other studies showed that resin cements provide good marginal integrity, especially in the occlusal margins, where adhesion is enhanced by the presence of a greater thickness of the enamel3. The concepts of adhesion and cementation were not designed exclusively for adhesive restorations and no protocols have been established that determine which cement works best for indirect restorations.
According to Corts & cols., 20134, Table Top occlusal restorations or overlays, are indirect restorations indicated to restore losses of dental hard tissues, mainly due to different types of non-carious lesions. In these cases, they recommend that the thickness of the restorations be at least 1.5 mm.
Restorations of resin materials placed indirectly, exhibit acceptable long-term clinical performance when rehabilitation of the posterior teeth is needed. However, failures occur after cementation and the selection of the best treatment protocol remains subjective. The available studies and their synthesis cannot provide reliable evidence in this field. For this reason, the present study sought to determine with which cementing agent decreases the degree of microfiltration that occurs when cementing the inlays of table top type ceromer.
Materials y methods
This experimental, randomized in vitro study was approved by the Research Ethics Subcommittee of the Central University of Ecuador (SEISH-UCE). The experimental part was carried out in the laboratories of the Faculty of Dentistry of the Central University of Ecuador.
36 intact human third molars were used, extracted by therapeutic indication, which were disinfected with 10% sodium hypochlorite solution and kept in saline at 37°C until the time of the experiment. The dental pieces were mounted on acrylic specimens so that the coronary portion is exposed and prepared from silicone matrices with Zhermak® addition silicone paste (Italy), to guide the preparation and occlusal wear. All the pieces were prepared standardized to receive table top type inlays4.
For the carving of the dental pieces, with the guide of matrices with silicone to standardize the procedure of wear (figure 1), the occlusal surface of each tooth was prepared using a high-speed hand piece (NSK, Japan) between 100,000 and 500,000 rpm with air-water spray and 1.5 mm round-cut, truncated cone-shaped diamond milling cutters (ISO544) were used and changed every 5 preparations.

Figure 1. Silicone guide used as a wear guide (1.5 mm).
The conformation of the occlusal box was carved out by wearing 1.5 mm, maintaining the morphology of the cusps (figure 1), After preparation, the finishing was done with Sof-Lex® (3M) discs, all edges were rounded and a smooth surface was obtained (figure 2).

Figure 2. Preparation and smoothing of the cavity.
After preparation, Elite Glass Zhermak® transparent silicone matrices (Italy) were used which were made together with the carving matrices, this type of addition silicone is specific for the creation of transparent matrices for aesthetic reconstructions in photopolymerizable composites, with direct or indirect technique.
The inlays were made with CERAMAGE® (SHOFU, Japan) directly on the samples, previously insulating was put and the resin was added with the help of the matrix. It was photocurred in the SolidiliteV® curing chamber (SHOFU, Japan) according to the manufacturer's instructions for 5 minutes. The inlays were polished and calibrated to 1.5 mm (figure 3).

Figure 3. CERAMAGE® photo curing process (left and center). 1.5 mm calibration (right).
All samples were stored in airtight boxes and kept at 37°C for 24 hours. Prior to the experiment, the inlays were sandblasted (Microetcher, USA) with aluminum oxide (Ortho Technology) of 50 microns for 15 seconds, 2 cm away, perpendicular to the inlay and 2.8 bar pressure, then irrigated with water and air dried.
Subsequently, the study population was randomly divided into 3 groups (n= 12), and randomly cemented with the 3 cements of the experiment, following the manufacturer's instructions. Randomly, 3 samples were chosen in each cementing process, alternating the placement of a different cement.
Group A: The surface of the teeth was disinfected with 0.5% sodium hypochlorite solution and washed for 10 seconds; it was dried with air application and then ortho phosphoric acid at 37% Scotchbond® (3M, USA) was applied, for 15 seconds in enamel, washed for 30 seconds, drying with absorbent paper towels. Each inlay was etched with 37% Scotchbond® orthophosphoric acid (3M, USA), for 1 minute, washed for 30 seconds, then air dried for 10 seconds and finally cemented using a self-etching RelyX® U200 cement (3M, USA), which was mixed manually in a block of waxed paper, with a plastic spatula, the paste was spread in the inlay to later settle on the tooth and was fixed with manual pressure to settle the incrustation in the correct position; excesses were removed and after 5 minutes glycerin was placed in the cementation interface and then light-cured using a Valo® brand Led Light Lamp (Ultradent, USA) with a standard power of 1000 Mw / cm2 for 20 seconds.
Group B: The surface of the teeth was disinfected with a 0.5% sodium hypochlorite solution, washed for 10 seconds, dried with air application and then for 15 seconds in enamel and 10 seconds in dentin ortho phosphoric acid at 37% Scotchbond® (3M, USA) was applied, it was washed for 30 seconds, drying with absorbent paper towels. Next, Singlebond® Universal (3M, USA) adhesive was placed, which we rubbed for 20 seconds with the help of a microbrush, it was dried for 5 seconds with an air jet and photopolymerization was continued using a Led Light lamp brand Valo® (Ultradent, USA) with a standard power of 1000 Mw / cm2 for 20 seconds. Each inlay was etched with orthophosphoric acid at 37% Scotchbond® (3M, USA) for 1 minute, washed for 30 seconds, and air dried for 10 seconds. The application of Singlebond® Universal adhesive (3M, USA) was continued and dried with an air jet for 5 seconds without photopolymerization. Finally it was cemented using a universal cement RelyX Ultimate® (3M, USA), it was mixed manually in a block of waxed paper, with a plastic spatula, the paste was spread in the inlay to later settle on the dental piece and it was fixed with manual pressure to settle the embedding in its correct position, excesses were removed and after 5 minutes glycerin was placed in the cementation interface and then light-cured using a Valo® Led Light Lamp (Ultradent, USA) with a standard power of 1000 Mw / cm2 for 20 seconds.
Group C: The conditioning and adhesive protocol was similar to group B, then Enamel Plus HRI® resin (Micerium, Italy) thermoplasticized at 55oC for 60 minutes was used to cement (figure 4A); the excesses were immediately removed, and glycerin was placed at the cementation interface, then light-cured using a Valo® Led Light Lamp (Ultradent, USA) with a standard power of 1000 Mw / cm2 for 20 seconds (figure 4B).

Figure 4A. A: Thermoplastification at 55°. B: Polymerization with Valo® lamp (Ultradent, USA).
All groups were polished using silicone rubber in decreasing order, for 30 seconds in both directions. The three groups were subjected to thermocycling for 3300 cycles, each cycle included 20 seconds at each temperature, that is to say at 5°C and 55°C, the samples were subsequently dried and two layers of transparent enamel were placed 1 mm away from the cementation interface. Finally, the samples were placed in a 2% methylene blue solution for 24 hours. Next, a cut was made in the mesio-distal direction of the crowns with the help of a micromotor at 40,000 rpm equipped with irrigation and a diamond disc Dupla face total brand Sorensen (Canada).
A stereo microscope SZ51 (Olympus, Japan) and a North Carolina periodontal probe Hu-Friedy (USA) calibrated every millimeter were used for the microfiltration observation process. Two observations were made: in the mesial and distal portion of all samples, obtaining 24 measurements per group.
The data was stored in a database in Excel, then the experimental values were archived and coded using the BioEstat 5.3 software. The relationship of the data with normality according to the Shapiro Wilk test did not show a homogeneous distribution (p = <0.05). Statistical analysis was performed using the non-parametric Kruskal Wallis test.
Results
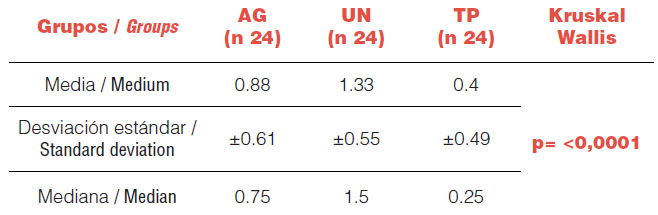
Table 1 shows the descriptive statistics in which the mean, medians and standard deviation of the results are presented. The statistical analysis was performed using the Kruskal-Wallis test, with a significance of 95% it determined the acceptance of the alternative hypothesis H0, in which it is determined that there are differences in the microfiltration of the groups (p= <0.05).
Table 1. Descriptive statistics. Ag: Self-etch cement; UN: universal cement; TP: thermoplastic resin.
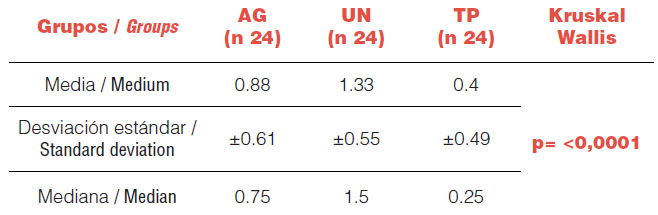
To establish what are the differences that exist between the groups, the Dunn comparison was carried out, a post hoc test for pairwise comparisons with a level of statistical significance of 95%.
Table 2. Comparison between pairs between groups. Cementation with thermoplastic resin has statistically lower values than other cements with a significance of 95%.

.
By means of the statistical analysis it was possible to determine that the degree of microfiltration was lower in the plasticized resin cement (p= <0.05) with a statistically significant difference with respect to the other cements. There was no difference between self-etch resin cements in relation to universal resin cement.
Discussion
Through this study, we sought to assess the marginal microfiltration in table top resins or overlays after cementation. The thermoplastic resin had the lowest values in the degree of microfiltration with an average of 0.4 mm; on the contrary, with the universal cement the highest values were obtained with an average of 1.33 mm, which was not significant in relation to the self-etch cement (0.88 mm). Through stereo microscope observation, it was possible to determine that in table top restorations the degree of microfiltration was lower when they were cemented with thermoplasticized resin (p= <0.05) with a statistically significant difference with respect to the other cements. There was no difference in microfiltration between self-etched resin cements in relation to universal resin cement.
Several authors agree that modern restorative dentistry is substantially adhesive. The preservation of healthy dental tissue has become a priority, including developing techniques and designs of ultraconservative preparations, such as the aesthetic clinical protocol (PIAR)5-6. In posterior pieces, the wear of the teeth has also been limited thanks to the development of new materials that allow a less aggressive carving, in the development of the present study, the design of the preparation was taken in account and was standardized in 1.5 mm, according to the characteristics of the material (CERAMAGE); however, there are reports of success with smaller thicknesses, but not in the long term4.
In the same way, in other studies they concluded that the posterior ultra-thin occlusal veneers of composite resin in CAD/CAM had a significantly greater fatigue resistance than those of ceramics, recommending its application even in the posterior teeth of patients with high load requirements7-8. Which corroborates the design of both the preparation and restoration, used in the present study.
Ultrafine occlusal veneers represent a conservative alternative to traditional techniques, they also allow only a strategic reduction of healthy dental structure or perhaps no preparation, dentists should ideally choose flat and circumferential designs to improve clinical performance and longevity, although other designs of preparations such as: occlusal veneers with circumferential shoulder line or occlusal veneers with intracoronal extension are also described9-10. However, studies in 2018 recommend designs of preparations such as those applied in this report, since these forms of preparation allow the dental technician to manufacture a well-adjusted and uniform thickness restoration and thus obtain a very low fracture and disunity rate1,11.
As for its maximum load capacity, minimally invasive occlusal veneers made of ceramic, hybrid or polymeric materials can be applied to correct the occlusal wear of the teeth with exposed dentin12. An evaluation of the clinical performance of indirect restorations was performed in 2019 by clinical examination, intraoral radiographs and clinical photographs. The general clinical evaluation aimed to confirm the absence or presence of caries or fracture of the restoration, while the quality of the restoration was judged in intraoral photographs. The status of restorations with respect to margins, anatomy and color was evaluated using three quality scores (A= ideal, B= satisfactory, C= insufficient). During this period of observation in the medium and long term, no clinical failure was reported. Only a few restorations (mainly those made with conventional nanohybrids) presented a discreet marginal discoloration or a change in occlusal anatomy due to wear. This first clinical survey with long-term follow-up supports the application of the aforementioned clinical concepts, which until now have only been validated by in vitro studies13.
A retrospective study in 2018, concluded that the indirect composite resin technique has a high long-term success rate, with a probability of survival at 10 years of 81%. The probability of survival at 20 years varies from 44% to 75%. Surviving restorations showed excellent preservation of clinical features (color, marginal discoloration, marginal adaptation, anatomical shape, surface roughness and secondary caries). The low incidence of secondary caries is associated with a good marginal seal that remains unchanged during the follow-up period14. One of the limitations of the present study is the number of cycles in the aging process; however, the objective was to determine microfiltration after cementation, without taking into account the longevity of the procedure; in other studies the durability of the material will be evaluated.
Angeletakia & cols., 201615; Through a systematic review and meta-analysis, they studied the clinical importance of resin composites, placed directly or indirectly, found promising long-term clinical performance when rehabilitation of the posterior teeth is needed. It guarantees the use of indirect resins as restorative material, which is one of the indications of the material used in the study; concordant with other studies where indirect inlays of adhesive composite resin showed acceptable long-term clinical results in terms of function, although surface and margin characteristics changed over time16.
Milutinovic & cols., 200717, in one study compared several types of cements, concluding that resin-based composite cement has the lowest porosity and all pores identified are smaller than 20 nm. So that in the present investigation it was used as cementing materials, resin-based cements.
In a first investigation carried out in 2010, RelyX Unicem® (3M) self-adhesive resin cement showed an acceptable clinical behavior after two years of clinical service. It seems clear that resin materials are indicated in the cementing of inlays with the study material, which is widely used in the clinic in the cost-benefit relationship with porcelains; the contribution of this research will help the clinician to choose the material for cementing subsequent indirect restorations.
According to Peumans & cols., 201018,19, selective etching of enamel before fixation had no significant influence on marginal integrity, tooth integrity, sensitivity or complications of restored teeth after 24 months. Later in 2013, in a continuation of the first investigation, they concluded that RelyX Unicem® self-adhesive cement can be recommended for joining ceramic inlays. After 4 years, they found an evident deterioration in marginal integrity, since only 5% of the restorations exhibited excellent marginal adaptation. In 90% of the restorations small marginal deficiencies were observed, still clinically acceptable. These results could be contrasted with the present study, since the self-etch cement obtained levels of microfiltration at the enamel level, despite having previously made a selective etching of the enamel; although not statistically superior to total engraving.
Melilli & cols., 2018³, evaluated three cements: Calibra® (Dentsply), Relyx® Unicem (3M) and Charisma® Flow (Kulzer) and found the highest microfiltration in fluid resin, especially in the cervical margins, suggest that the authors advocate that Cements created to cement, are used for that purpose. These results contrast with our study that found less filtration in the resin material, in this case thermoplasticized, new studies should compare these two materials.
It is important to note that bond strengths vary between specific cements, but total etch cements generally provide the highest retention and self-adhesive cements can provide a bond strength almost equal to self-etch systems, which matches the results presented in this report. High bond strengths can be achieved with self-adhesive resin cements in non-retentive teeth. The result of this review of self-adhesive resin cements would suggest that these materials may show clinical performance similar to other dental cements based on resins and non-resins20.
It is evident that thermocycling has a greater impact on adhesion behavior than water storage21, which is why it was chosen in the methodology for our study; However, it is necessary to emphasize that the objective was to evaluate microfiltration after cementation and not longevity, which should be evaluated with studies that have a longer aging process.
Victoria & cols., 201322, analyzed that the surface treatment of the indirect resin compound with silane followed by a bonding agent (adhesive) did not affect the resistance of dentin binding. The self-adhesive resin cements tested obtained less microtraction values than the RelyX® ARC total etch resin cement. It agrees with our study, although our research was focused on microfiltration.
Self-etched adhesive systems reduce the time spent in clinical practice. However, at the interface they behave like permeable membranes, which facilitates the passage of fluids from the oral environment to dentin and vice versa, being more susceptible to degradation. In addition, its use is limited when dual and self-curing cements are use, as their components may interfere with the polymerization process. They are also prone to form a discontinuous, irregular and shallow hybrid layer associated with low wettability, system viscosity and low infiltration in dental tissues23. Self-etch adhesives were not used in our experiment; the results of Abad & cols., 201923, can be applied to other investigations that evaluate their behavior with universal and thermoplastic resin cements.
Sampaio & cols., 201624, evaluated the volumetric polymerization contraction and the film thickness of several cementation techniques using three-dimensional microcomputed tomography, concluding that: the volumetric polymerization contraction of the preheated direct restorative composite resins was significantly greater than that of coating cements or fluid composite resins. As the volumetric shrinkage of polymerization of the resins is greater, these can generate an interface which would result in greater microfiltration which was not evidenced in the results obtained in the present investigation. However, Bucheli & Mena, 20172, concluded that the technique of cementation with thermo-plasticized resin showed less marginal microfiltration, while the technique that presented the greatest marginal microfiltration was cemented with the self-adhesive dual cement. New in vitro and controlled clinical studies should clarify this controversy.
In conclusion, conventional thermoplastic composites seem to be a potential alternative for cementing indirect restorations in the posterior sector, where microfiltration is a relevant complication.
Conclusions
Through this study, it was possible to determine that the degree of microfiltration was lower in plasticized resin cement with a statistically significant difference from the other cements (p = <0.05). There was no difference between self-etch resin cements in relation to universal resin cement.
Interests conflict
The authors declare no conflict of interest in the presentation of data, preparation and publication of this article.
Bibliografía
- Angerame D, De Biasi M, Agostinetto , Franzo A, Marchesi G. Influence of preparation designs on marginal adaptation and failure load of full-coverage occlusal veneers after thermomechanical aging simulation. Journal Esthetic Restorative Dent. 2019 May; 31(3): p. 280-289.
- Bucheli Romero MDC, Mena Córdova N. Evaluación de la microfiltración en restauraciones indirectas cementadas con resina precalentada, cemento de grabado total y un agente auto adhesivo. Tesis (Especialista en Rehabilitación Oral). Quito: Universidad San Francisco de Quito, Colegio de Posgrados; 2017. Report No.: http://repositorio.usfq.edu.ec/handle/23000/6432.
- Melilli D, Cumbo E, Baldissara P, Wandscher V, Valandro L, Gallina G, et al. Evaluation of marginal leakage after mechanical fatigue cycling of composite inlays luted with different cements. Academy of General Dentistry. 2018 Julio.
- Corts J, Arrospide L, Cedrés C, Corallo L. Restauraciones de cerámica adherida. Continuum Restaurador Posterior. Actas Odontológicas. 2013 Julio; X(1): p. 16-27.
- Veneziani M. Posterior indirect adhesive restorations: updated indications and the Morphology Driven Preparation Technique. The International Journal of Estheticdentistry. 2017; 12(2).
- Ferraris F. Posterior indirect adhesive restorations (PIAR): preparation designs and adhesthetics clinical protocol. The International Journal of Estetic Dentistry. 2017; 12(4).
- Magne P. In Vitro Fatigue Resistance of CAD/CAM composite resin and ceramic posterior occlusal veneers. Journal of Prosthetic Dentistry. 2010 Septiembre; 104(1).
- Luis Schlichting HPBPM. Novel-design ultra-thin CAD/CAM composite resin and ceramic occlusal veneers for the treatment of severe dental erosion. Journal of Prosthetic Dentistry. 2011 Abril; 105(4): p. 217-26.
- Schlichting , Holz Resende T, Rodriguez Reis K, Magne P. Simplified treatment of severe dental erosion with ultrathin CAD-CAM composite occlusal veneers and anterior bilaminar veneers. Journal Prosthet Dent. 2016 Oct; 116(4): p. 474-482.
- Kotb S, Shaker A, Halim C. Fatigue resistance and 3D finite element analysis of machine-milled ceramic occlusal veneers with new preparation designs versus conventional design: an in vitro study. Department of Fixed Prosthodontics, Faculty of Dentistry Cairo University. 2019 Julio.
- Politano G, Van Meerbeek , Peumans M. Nonretentive Bonded Ceramic Partial Crowns: Concept and Simplified Protocol for Long-lasting Dental Restorations. Journal Adhesive Dent. 2018 Diciembre .
- Maeder M, Pasic P, Adreas E, Mutlu , Goran B, Loannidis A. Load-bearing capacities of ultra-thin occlusal veneers bonded to dentin. Journal of the Mechanical Behavior of Biomedical Materials. 2019 Julio; 95(1): p. 165-171.
- Dietschi D, Spreafico R. Evidence-based concepts and procedures for bonded inlays and onlays. Part III. A case series with long- term clinical results and follow-up. The International Journal of Esthetic Dentistry. 2019 118-133; 14(2).
- Ravasini Francesco DBMPTRPOM. reatment Outcome of Posterior Composite Indirect Restorations: A Retrospective 20-Year Analysis of 525 Cases with a Mean Follow-up of 87 Months. International Journal Periodontics Restorative Dentistry. 2018 Sep; 38(5): p. 655-663.
- Angeletakia F, Gkogkosb A, Papazoglouc E, Kloukosd D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. Journal of Dentistry. 2016 Oct; 56(1): p. 12-21.
- Derchi , Marchio V, Borgia V, Ozcan M, Giuca R, Barone. 12-year longitudinal clinical evaluation of bonded indirect composite resin inlays. Quintessence International. 2019 Ene; 50(1).
- Milutinovic Nikolic A, Medic V, Vukovic Z. Porosity of different dental luting cements. Dental Materials. 2007 Jun; 23(6): p. 674-8.
- Peumans M, De Munk J, Van Landuyt K, Poitevin A, Lambrechts P, Van Meerbeek B. Two-year Clinical Evaluation of a Self-adhesive Luting Agent for Ceramic Inlays. Journal Adhesive Dent. 2010 Apr; 12(2): p. 151-61.
- Peumans M, De Munck V, Van L, Van E, Van M. Four-year clinical evaluation of a self-adhesive luting agent for ceramic inlays. Clinical Oral Invest. 2013 Apr; 17(3): p. 739-50.
- Stamatacos C, Simon J. Cementation of Indirect Restorations: An Overview of Resin Cements. Compendium of continuing education in dentistry. 2013 Apr; 34(1): p. 42-6.
- Spitznagel F, Horvath , Guess P, Blatz M. Resin Bond to Indirect Composite and New Ceramic/Polymer Materials: A Review of the Literature. Journal of Estheticand Restorative Dentistry. 2014 Dec; 26(6): p. 382-93.
- Victoria Fuentes M, Sanz Ceballos L, González-López S. Bond strength of self-adhesive resin cements to different treated indirect composites. Clinical Oral Investigations. 2013 April; 17(3): p. 717–724.
- Abad Coronel C, Naranjo B, Valdiviezo P. Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature. Journal Dent (Basel). 2019 Jul; 7(3): p. e71.
- Sampaio , Malta J, Cáceres E, Rigo , Coelho P, Bonfante E, et al. Volumetric shrinkage and film thickness of cementation materials for veneers: An in vitro 3D microcomputed tomography analysis. Journal Prosthetic Dent. 2016 Jun; 117(6): p. 784-791.

Reconocimiento-NoComercial-CompartirIgual
CC BY-NC-SA
Esta licencia permite a otros entremezclar, ajustar y construir a partir de su obra con fines no comerciales, siempre y cuando le reconozcan la autorÍa y sus nuevas creaciones estÉn bajo una licencia con los mismos tÉrminos.