Cerámicas: una actualización
Ceramics: an update
Cerâmica: uma atualização
Marcelo Cascante Calderón1,2, Inés Villacís Altamirano1,2, Igor Studart Medeiros3
RECIBIDO: 18/12/2018 ACEPTADO: 29/03/2019 PUBLICADO: 31/07/2019
- Postgraduate PhD Program of Biomaterials and Oral Biology, School of Dentistry, University of São Paulo (USP), São Paulo, SP, Brazil.
- Facultad de Odontología, Universidad Central del Ecuador, Quito, Ecuador.
- Department of Biomaterials and Oral Biology, School of Dentistry, University of São Paulo (USP), São Paulo, SP, Brazil.
CORRESPONDENCIA
Marcelo Cascante Calderón
Facultad de Odontología.
Universidad Central del Ecuador.
mcascante@uce.edu.ec
RESUMEN
Las cerámicas dentales utilizadas para restaurar y reemplazar tejido dental perdido de los dientes o las piezas dentales mismas, han sufrido una enorme transformación desde que aparecieron las primeras porcelanas hace ya varias décadas. Con las feldespáticas se podían hacer dientes, coronas y puentes, pero necesitaban un soporte de metal para que no sufran fracturas con los esfuerzos masticatorios, y por ello no tenían una apariencia vital. Hoy en día, han aparecido muchas otras cerámicas con diferentes y mejoradas características mecánicas y ópticas, lo que ha permitido que los odontólogos puedan por primera vez ofrecer a sus pacientes dientes artificiales con sorprendente naturalidad. Objetivo: Describir la clasificación actual, las características mecánicas y ópticas, así como la microestructura y los usos clínicos de las diferentes cerámicas dentales utilizadas hoy en día. Materiales y métodos: Revisión de la literatura acerca del tema, en tres de los más importantes buscadores de internet (Pubmed, Cochrane, Web of Science). Limitando su busqueda a artículos en inglés y publicados en los journals de investigación de materiales dentales con calificación Q1 y Q2. Resultados: Se revisaron 69 artículos publicados entre 1975 y 2019 los cuales aportaron una fuente interesante de información que permitió desarrollar el conocimiento acerca de la clasificación, microestructura, propiedades mecánicas y ópticas, usos clínicos y forma de procesamiento de las cerámicas. Conclusiones: Actualmente los odontólogos tienen a disposición una amplia variedad de materiales cerámicos con diferentes composiciones y características únicas que son necesarias conocer al momento de escoger la cerámica específica para cada necesidad de los pacientes.
Palabras clave: Porcelana dental; cerámica; restauraciones de cerámica; silicatos de aluminio; circonio; vita enamic.
ABSTRACT
The dental ceramics used to restore and replace lost tooth tissue or the teeth have undergone a huge transformation since the first porcelains appeared several decades ago. With the feldspathic teeth, crowns and bridges could be made but, they needed a metal support so that they did not suffer fractures with the masticatory efforts, and therefore they did not have a vital appearance. Today, many other ceramics with different and improved mechanical and optical characteristics have appeared, which has allowed dentists to offer artificial teeth to their patients for the first time with surprising naturalness. Objective: Describe the current classification, mechanical and optical characteristics, as well as the microstructure and clinical uses of the different dental ceramics used today. Materials and methods: Review about the literature on the subject, in three of the most important internet search engines (Pubmed, Cochrane, Web of Science). Limiting your search to articles in English and published in the journals of research of dental materials with qualification Q1 and Q2. Results: 69 articles published between 1975 and 2019 were reviewed, which provided an interesting source of information that allowed the development of knowledge about classification, microstructure, mechanical and optical properties, clinical uses and method of processing ceramics. Conclusions: Currently, dentists have available a wide variety of ceramic materials with different compositions and unique characteristics that are necessary to know when choosing the specific ceramic for each patient need.
Keywords: Dental porcelain; ceramics; ceramic restorations; aluminum silicates; zirconium; vita enamic.
RESUMO
A cerâmica dentária usada para restaurar e substituir o tecido dentário perdido ou as próprias peças dentárias sofreram uma enorme transformação desde que as primeiras porcelanas surgiram várias décadas atrás. Com os materiais feldespáticos, podiam ser feitas coroas e pontes, mas eles precisavam de um suporte de metal para não sofrer fraturas com os esforços mastigatórios e, portanto, não tinham uma aparência de vitalidade. Hoje, outras cerâmicas com características mecânicas e ópticas diferentes e aprimoradas surgiram, o que permitiu aos dentistas oferecer dentes artificiais a seus pacientes pela primeira vez com uma naturalidade surpreendente. Objetivo: Descrever a classificação atual, características mecânicas e ópticas, bem como a microestrutura e os usos clínicos das diferentes cerâmicas odontológicas utilizadas atualmente. Materiais e métodos: Revisão da literatura sobre o assunto, em três dos mais importantes mecanismos de busca na Internet (Pubmed, Cochrane, Web of Science). Limitando a sua pesquisa a artigos em inglês e publicados nas revistas científicas de materiais dentários com qualificação Q1 e Q2. Resultados: Foram revisados 69 artigos publicados entre 1975 e 2019, que forneceram uma fonte interessante de informações que permitiram desenvolver conhecimento sobre a classificação, microestrutura, propriedades mecânicas e ópticas, usos clínicos e forma de processamento da cerâmica. Conclusões: Atualmente, os dentistas têm disponível uma ampla variedade de materiais cerâmicos com composição diferente e características únicas que são necessárias conhecer ao escolher a cerâmica específica para cada necessidade do paciente.
Palavras-chave: Restaurações cerâmicas; silicatos de alumínio; zircônio; vita enamic.
INTRODUCTION
Since the successful introduction of the first feldspathic ceramic with metal backing for dental use developed by Weistein in 19601 ceramics have undergone a great evolution with the aim of recovering and replacing lost dental structures, such as enamel and dentin, by various causes.
In the US in the early 90 about 35 million people used porcelain dental crowns1. In Ecuador we do not have epidemiological data but it is estimated that thousands of people must have at least one dental crown and that number will surely increase.
This article aims to briefly and concisely describe the current classification, mechanical and optical characteristics, as well as the microstructure and clinical uses of the different dental ceramics used today.
The term ceramic comes from the Greek keramiké which means "burnt clay".
Ceramics are defined as materials formed by the union of metallic elements such as: Al, Li, Ca, Mg, K, Ti, Zr, and nonmetals such as O, B, F2,3.
Dental ceramics are basically composed of metal oxides that, combined or alone, are sintered at high temperatures to obtain a solid piece, with a reduced number of pores and mechanically resistant. Depending on the types and proportions of metal oxides, the microstructure obtained after sintering can be totally crystalline, vitro-ceramic or predominantly vitreous.
This microstructure provides the optical properties (fluorescence, translucency / opacity and opalescence) and mechanical properties (wear resistance, hardness, flexural strength)4.
Due to the type of bond and its microstructure, this material is chemically inert and therefore biocompatible; It has high values of compressive strength, hardness, and fundamentally when treated with colors and pigments it can resemble the natural appearance of the tooth, it is highly appreciated by dentists, technicians and patients to rehabilitate lost dental tissues5.
However, they are fragile and are not able to deform plastically, have a high modulus of elasticity and with only a deformation of 0.01% can experience catastrophic fractures.
Another of the disadvantages of ceramics is that due to their high hardness values they are capable of causing wear of the opposing teeth, especially when they are not well polished or glazed2.
Current classification
Ceramics are currently classified according to their microstructural composition and their ability to react to acid attack in:
- Vitreous ceramics composed mainly of silica (feldspathic): sensitive acids
- Vitreous ceramics composed of silica but with filler crystals (leucite and lithium disilicate, lithium silicate): sensitive acids
- Polycrystalline ceramics (Zirconia): acid resistant3,6.
Feldespatic ceramics or dental porcelains
Feldspathic ceramics come from a rocky mineral called feldspar, which is very abundant in nature and whose main composition is silica, and other minerals such as quartz, kaolin and clay.
In order to use feldspar (Na2O/K2O.Al2O3.6SiO2) as a raw material in the manufacture of porcelain it is necessary to remove iron as a pollutant from its composition through certain chemical processes, mix it with quartz and submit it to high temperatures (13000C). At this temperature there is a unique phenomenon known as "incongruous fusion" in which the vitreous phase is formed, and inside it the leucite crystals begin to grow, but in a scattered way inside2.
The manufacturers then submit this dough to an abrupt cooling of it which produces a fracture in several pieces called "frita". These pieces of frit are subjected to a grinding process in large mills of zirconium balls, for several weeks until obtaining a fine and delicate powder to which metal oxide pigments will be added to provide the colors similar to the natural tooth.
This final powder will be mixed with a liquid, by the prosthetic to perform the modeling of the dental piece2.
Due to the vitreous phase is present in about 75 to 85% of the total volume of this porcelain and the crystals represent only 15 to 25% of the total, these are called vitreous or simply vitreous ceramic ceramics3,6,7.
Meanwhile, due to the fact that hydrofluoric acid (HF) is capable of dissolving the vitreous matrix and exposing crystals of the crystalline phase8,9, which produces a very suitable irregular surface to improve the wettability of an agent. bonding8,10, this porcelain is also called acid-weak.
Mechanical and optical properties
In general, dental porcelains, like other ceramics, unlike metals, have a poor ability to absorb large amounts of energy before suffering a catastrophic fracture.
The feldspathic are the weakest (least resistant) of all because they have a large percentage of vitreous phase inside and very little crystalline phase. Fracture toughness (KIC) and low tensile strength are directly related to this phenomenon. In other words, the lower the leucite content, the lower KIC and vice versa. César. et al, report low values between 0.71 and 0.75 KIC in porcelains with 0% leucite content, while having higher values of between 1.22 and 1.23% KIC in porcelains with 22 and 23% of leucite11. Other research papers show similar values of KIC12-16.
This is due to the fact that in a vitreous matrix the presence of defects, intrinsic failures, or microcraks produced during the phase of abrupt cooling when they are processed, or included at the time of manufacturing the dental pieces, when subjected to forces or masticatory stress they spread without any obstacle in their path until the material breaks.
While in a porcelain reinforced with crystalline phase, the presence of leucite crystals opposes the progress of a defect, or even compresses it, stopping its passage and improving its mechanical resistance to fracture12.
For this reason feldspathic porcelains need an internal structure of a material with a high KIC such as the remanescent dental structure itself, metals or other ceramics, in order to survive in the mouth without risk of damage or breakage.
As for their optical properties, feldspaths with a large volume of vitreous matrix, let the light in and consequently are translucent, but the higher the content of leucite crystals, the light will collide with them and deviate with what will be more opaque.
It is well known that the increase of certain oxides and dusts allows dental restorations of great similarity to the color of the tooth, and even the gum.
Feldspathic porcelains are composed of two phases: a vitreous phase or matrix and a crystalline phase, made up of leucite crystals. Said crystals can have a length of between 5 to 10 µm and are very similar to the extensions of a dendrite16.
Catell et, al found a high proportion (7-10%) of spherical or micropore defects within the vitreous phase and in the vicinity of the leucite crystals, which would appear to act as stress detonators when subjected to stress-causing forces. internal This would explain its low fracture and tensile strength13.
Such pores would form at the time of the sudden cooling of the frit mass when the porcelain powder is manufactured.
Clinical uses
Crowns and bridges of up to 3 metal-porcelain units, for which the manufacturers of porcelain powders adjust the linear thermal expansion coefficient (LTEC) of the ceramic to the metal by adding leucite, in order to prevent a great difference in the LTEC produces areas of stress concentration and therefore fractures of the material, during cooling.
While the dental technician submits the metal alloy infrastructure to a pretreatment of metal oxidation so that a chemical bond between them occurs2.
Inlays, metal-free porcelain onlays. Although it seems a contradiction to everything we have been trying until now, the development of modern techniques and adhesives has allowed the adhesion between porcelains and enamel to be very reliable and optimal in order to resist the forces of chewing17.
Facets or veneers of pure porcelain. Clinical trials show that the survival rates of these restorations are between 82 and 96% after 10 to 21 years17,18 as long as they have been prepared and cemented in enamel exclusively19 when the preparation and carved exposed 50% or more dentin were found more failure due to detachment and fracture. As reported by Beier et al., in 2012.
Processing
Dental restorations based on feldspathic porcelain can be obtained by sintering, injection and CAD CAM.

Figure 1. Dental crown in ceramic metal.
Note: the opacity of the cervical metal backing, due to the great translucency of feldspathic ceramics.
Leucita
One of the main leucite-based ceramics was presented in 1991 under the name of IPS Empress Ceramic. (Ivoclar Vivadent, Leichtenstein). It belongs to the group of vitreous ceramics and therefore they are also weak acids, but unlike the previous one, it has a high percentage of crystalline phase in the form of leucite crystals. These crystals are added by the manufacturer through the addition of a synthetic feldspar powder (K2O,Al2O3,6SiO2)20. And also the manufacturers are able to control the quantity and quality of the crystals by means of various treatments.
The proportion of leucite crystals in the crystalline phase can vary from 22 to 50% in these porcelains while the vitreous phase is formed of a silicate aluminum glass3.
The differences between these percentages of the leucite content may be induced by various factors including: multiple porcelain firing21, heat treatments22, cooling, and even long exposures to saliva make the porcelain mature and contain higher percentage of leucite23.
Research shows that a percentage of leucite between 20 and 30% is able to improve the mechanical properties of this porcelain24, 25, while at a higher percentage between 30 and 50% these properties do not increase significantly11.
Mechanical and optical properties
The mechanical properties of leucite, as well as feldspathic, are influenced by the differences between the coefficients of thermal expansion of leucite crystals and the crystalline phase, during cooling of the same at the time of being produced.
However, this procedure can produce microcracks inside the material, mainly due to the fact that there is much difference between the thermal expansion of a glassy phase and a crystalline phase, tensions are formed between them that can trigger cracks or defects due to thermal stress, which can lead to a fracture of the material when subjected to mechanical stress.
In fact, Kon et al., observed, by means of the scanning electron microscope, the formation of microcracks around the ends of the tips of the leucite crystals, and that these were enlarging when a higher percentage of leucite was present25.
Regarding its hardness (Vickers HV hardness), 450 HV values have been reported in porcelains with a leucite percentage of 20 to 50%. While other feldspathic porcelains with higher leucite values decrease the same between 350 and 400 HV25.
In what has to do with flexural strength, leucite reaches values of 81 MPa, unlike feldspathic porcelains that have much lower values.
Kon et al., reported that when the percentages of leucite are beyond 50% mechanical properties, they worsen.
As for its optical properties; Due to the better distribution of leucite crystals within the vitreous hue, the translucency is excellent because the light can pass through it very easily, however it has been observed that this property decreases as the thickness of the material26.
Microstructure
They have a microstructure very similar to that described for feldspathic, that is to say they have a vitreous matrix with leucite crystals inside, only that in these ceramics, the crystals are more homogeneously distributed inside, this is because the leucite It is added in powder form at the time of production, and by means of heat treatments manufacturers are able to control the growth and quality of these crystals.
Clinical uses
Ceramic metal prostheses of up to 3 units, metal-porcelain crowns27 inlays, onlays, coating of metal or other ceramic infrastructures, either vitreous or crystalline, veneers and contact lens type facets27. With very good results of durability in the medium term (8 years) but with serious risks of suffering fractures after 10 years of clinical use in the mouth28.
Processing
Dental restorations based on leucite can be obtained through various methods such as sintering, injection and CAD CAM.
Vitro-ceramic (lithium disilicate, lithium silicate with zirconia)
A material that has evolved a lot and currently stands out in dentistry is lithium disilicate, lithium silicate with zirconia or better known as vitro-ceramics.
These materials combine favorable optical characteristics with intermediate mechanical resistance, when compared to other dental ceramics.
Lithium disilicate (LS2) is classified as a vitreous ceramic but with particles and lithium disilicate crystals as filler. Therefore they are also considered acid-weak.
They were presented for the first time on the market in the early 90 under the trade name of IPS EMPRESS 2 (Ivoclar Vivadent, Shaan, Liechestein)29 and was composed of 65% needles or lithium disilicate crystals immersed in a glass mass with 1% porosity30, 31.
Currently, they were replaced by the e.max Press and e.max CAD system. Although the value of its porosity is low, Zarone et al, found that it can be a decisive factor and influence the hardness of the material, decrease its fracture toughness by up to 50%, especially when there is no perfect adaptation between the disilicate and the dental substrate; a correct cementation technique has not been performed, or there has been a wear of the ceramic piece after cementation.
The lithium disilicate crystals can be added by the manufacturer by means of the precise control of the composition of the glass, subjecting a thermal treatment to the mass thereof that causes the precipitation and growth of the crystals within it. Since both phases derive from glass, it is logical to think that the entire mass is altered during this process, which is called "ceramization"27.
Mechanical and optical properties
This ceramic, like the previous ones, has little tolerance for permanent deformation, they are unable to deform plastically, which makes them fragile materials. However, in recent years, manufacturers have made improvements to the ceramization process and the CAD CAM process by introducing pre-crystallized blocks (IPS e.max CAD, Ivoclar Vivadent) with a 40% percentage of lithium metasilicate (Li2Si2O5) available in different degrees of translucency and colors. These blocks are subjected to the carving of the piece inside the CAD CAM and then be heated at 840-8500C for 10 minutes which produces a precipitate of metasilicate that evolves in lithium disilicate (70%)32 which reaches a Flexural strength from 360 MPa to 400 MPa33,34 which is two or three times the value of feldspathic and Leukitic porcelains, which makes it a material with better characteristics than the previous ones35.
Despite having high values of resistance to fracture and flexion, the disilicate still does not tolerate major deformations or the presence of irregularities that are subjected to stress. Which means clinically that once the intraoral adjustments are cemented, they must be done with enough care to avoid excessive production of defects that can result in the reduction of the fracture resistance of the piece.
In addition, finishing and polishing are essential stages to ensure longer duration of the cemented piece.
As for its optical properties, it can be affirmed that the disilicate can be more translucent depending on the glassy phase present, or more opaque depending on the size and quantity of crystals. Manufacturers have been able to provide a wide range of colors and shadows that even can be combined with metallic dyes and oxides so that dental technicians and dentists can match the natural color of the teeth.
A last property different from that the other ceramics is its biocompatibility.
In fact, favorable reactions of soft and hard dental tissues of the mouth have been observed against the use of disilicate. Foster et al., 2014, presented the results of an investigation in which observed that this ceramic material allowed the development and growth of fibroblasts, mainly due to its microscopic granular structure that allows it to have micro spaces between its molecules which would allow the overlapping of extensions cell between them36, which can be corroborated in alive observations since there have been no inflammatory reactions in the soft tissues surrounding the crowns and ceramic restorations of these materials in patients who are using them.
Unlike inflamed tissues that have been seen in hundreds of patients using crowns and bridges made of metal-porcelain or other restorative polymers.
Microstructure
They have a 30% vitreous phase (SiO2,K2O, MgO, Al2O3,P2O5) and 70% of crystals mainly in the form of microscopic needles of lithium disilicate (Li2Si2O5) cross-linked between them37 and in turn submerged within the vitreous matrix.
Such microscopic crystals would be between 5 and 6 µm long and 0.5 to 0.8 µm thick38. The quality of these crystals has made this ceramic gain in resistance to fracture because these crystals are capable of demanding to deflect the advance of a microfissure in its passage through the interior of the ceramic making it retard and therefore more difficult produce its break.
Clinical uses
Lithium disilicate ceramics can be used for the fabrication of veneers and aesthetic facets on anterior teeth, inlays, onlays, unitary crowns without metal backing both in the internal sector and in the back sector with very good and lasting results.
Success rates of between 70 to 91% and survival of up to 10 years have been reported39,40.
Bridges of up to three units for replacement of previous parts and up to 1 premolar, it is not advisable to replace molars.
Processing
Dental restorations based on disilicate can be obtained by means of injection laboratory procedures and CAD CAM.

Figure 2. Lithium disilicate crown piece 13.
Note: The contrast with the metal-porcelain crowns of parts 11 and 21. As well as gingival inflammation after years of use.
Polycrystalline ceramics
Polycrystalline ceramics don’t have a vitreous phase, but they only have an internal crystalline structure, whose granules are very close and tight together, which makes them the owners of a hardness and fracture resistance superior to the previous ceramics.
Zirconia and alumina are the ceramic representatives of this group, however, due to the best mechanical properties, zirconia has been gaining more space within dentistry, in the last ten years, to the point that Alumina is no longer manufactured.
Tetragonal zirconia stabilized by ítria (Y-TZP)
Zirconium oxide or zirconia (ZRO2) has been known for centuries by Persians and Arabs who called it ZARGON, a Persian word that is formed from two ZAR words that means gold and GUM that means color.
Due to its extreme hardness and wear resistance it was used and used until today in heavy industry, to manufacture tools for cutting other materials such as rocks, metals, in civil industry, in the manufacture of electrical resistors of large thermal power plants, in chemical and mechanical industries41.
In the 70s, it began to be introduced in the medical field, as a biomaterial, but it was not until 1988 in a scientific article by Christel et al., that it describes for the first time its successful use in the replacement of worn femur heads in patients with hip problems 42. This success was mainly due to the high wear resistance of this material, when compared to the titanium used until then in this type of treatment. And its biocompatibility being unable to produce inflammatory reactions in the bone and muscle tissues of patients.
The entrance of zirconia to dentistry occurred about fifteen years ago43, mainly due to the pressure of dentists and people to be able to replace lost teeth with materials that were not metallic and that looked the same as natural teeth and that are able to resist the forces and the masticatory wear.
Zirconia has three known allotropic forms: the monoclinic form (M) is at room temperature, with the increase in temperature to 11700C it becomes tetragonal (T) while temperatures greater than 23700C become cubic (C) Its melting point is found at 27160C44-46.
To further increase its mechanical strength, the scientists added small amounts of certain metal oxides such as Itrium in proportions of up to 3-4%, stabilizing its state in the tetragonal phase, that’s why it is known as Partially Stabilized Zirconia by Itria, or Y-TZP41.
Unlike all previous ceramics, the latter does not present any glass phase or matrix, therefore it would no longer be weak-acid, but rather belongs to the group of resistant-acid. In which the attack with hydrofluoric acid (HF) has no reason to be47-49.
Due to its excellent mechanical properties, it has been called steel ceramic50. And because of its zero ion exchange, it is said to be chemically inert, which makes it perfect for dental restorations that do not cause irritation or damage to dental tissues51.
Some of the most representative trademarks of zirconia are: In-Ceram Zirconia (IZ) (Vita Zahnfabrik, Bad Sackingen, Germany), DC Zirkon (DZ) (DCS Dental AG, Allschwil, Switzerland) and Lava Plus (3M ESPE, St.Paul , MN; USA).
Among the most interesting mechanical properties are its high fracture toughness between 7 to 10 MPa.m1 / 2, its flexural strength between 680 to 1200 Mpa, its elastic modulus, similar to some 240 GPa metal alloys and a hardness of 13 GPa52, higher values up to 5 or 6 times more than the other ceramics.
While it has granules of zirconia in the form of fine particles that vary in size and can have less than 1 µ thick and agglomerated together by their edges leaving spaces of less than 0.3 µ or less where porosities that barely add up to 1 are located % or less of its total volume52. Which explains its high hardness.
The Y-TZP is considered an intelligent material because it is able to prevent a microfracture from advancing through the thickness of your body when it is under stress and ends up breaking it.
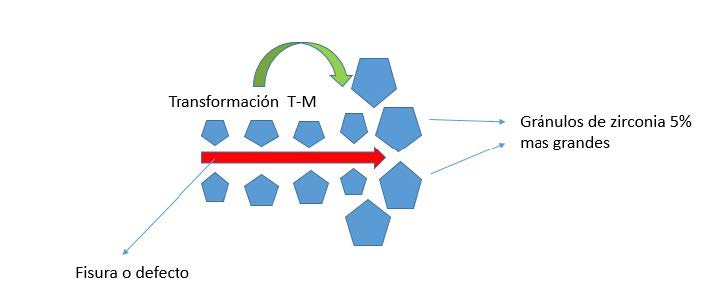
This phenomenon is due to the fact that when a fissure or defect is present on its surface, stabilized zirconia crystals change from tetragonal to monoclinic; with each change of state their granules increase in volume by 4 to 5% producing a compression effect on the fissure, hindering the advance of this53(figure 3).
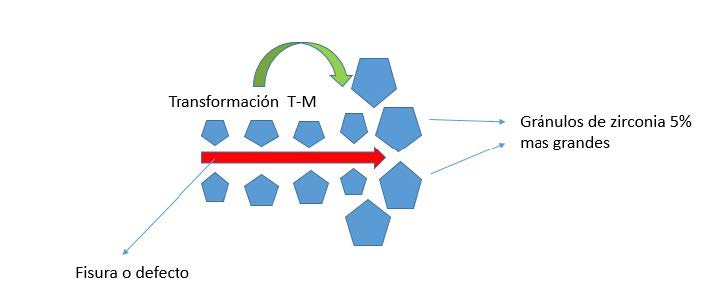
Figure 3. Shows the transformation of the tetragonal phase for Y-YTZP monoclinic when experiencing the presence of a defect (in red) induced by an external factor, which produces an increase in the volume of zirconia crystals by 5% which they increase the pressure on the fissure, hindering its advance.
As for its optical properties, it has an opaque white color because the granules are very cohesive with each other. What hinders the passage of light, so it is not reflected and less transmitted through its thickness, producing a great effect of dispersion of it.
Research states that compared to lithium disilicate, Y-TZP only has a translucency of 70%54,55.
However, the characteristic white color of it makes it very useful when wanting to match the color of natural teeth.
Recently, researchers have proposed alterations of the totally ceramic pieces in zirconia with reduced granule size and an increase in the cubic phase that returns to the more translucent zirconia.
Due to its chemical inertia, many researchers suggest carrying out treatments on the internal surface of it to improve its adhesion. Treatments such as tribochemical sandblasting (Cojet System or Rocatec 3M ESPE, St.Paul, MN; USA) is currently the gold standard when adhering with resinous cements is treated56-58.
Due to the oxygen layer that contaminates its surface, adhesive systems containing acid-phosphated monomers, particularly the MDP that has been shown to be able to chemically bond to its surface59-61, are being used with great success.
Microstructure
It is composed of crystals in the form of granules of tetragonal form, which is known as the tetragonal metastable phase (T) these granules are stable at room temperature because manufacturers add 2-5% mol% of Itria oxide (Y2O3)44.
Due to the absence of silica in its internal structure, it does not have an ion exchange62, which is why it is not possible to perform an acid etch with HF when trying to make an adhesion procedure.
Clinical uses
Due to its excellent mechanical and optical properties, extensive prosthetic restorations, bridges of more than 3 units, crowns and prostheses on implants, implants, orthodontic brackets, endodontic posts, inlays and onlays can be made.
Processing
Restorations can be obtained through CAD CAM procedures, followed by sintering.

Figure 4. Y-TZP bridge covered with feldspathic ceramic (VM9) of pieces 32-42 showing very good integration and aesthetics with its neighboring teeth.
Hybrid ceramics (differentiated and special composites)
The development of CAD CAM in recent years has also allowed the search and evolution of new ceramic materials capable of compensating for some of the deficiencies in the mechanical and physical properties of current ceramics.
As we have seen so far, the various ceramic materials are essentially inorganic, which carry in their internal composition various proportions of vitreous and/or crystalline phases that provide them with different degrees of hardness, fracture resistance, wear resistance, as well as different levels of translucency, opalescence and fluorescence.
However, it is not always possible to find a ceramic with the ideal properties, for example a zirconia with a high crystalline content will be harder and resistant to fracture than the others, but instead it will be more difficult to cement. A feldspathic, which can have great optical properties, but if it is not well polished, it can have a high wear potential of the opposing teeth.
The composites have been used for decades for the aesthetic restoration of decayed teeth, or fractured with excellent results. However, there are still many problems with them, especially the contraction they suffer during polymerization, poor mechanical properties and poor wear resistance63.
This has led many researchers around the world to develop a material that combines the best of these two elements so that it becomes a new alternative when restoring teeth.
The VITA company launched in 2011, a material called VITA ENAMIC (Zahnfabrik, Bad Säckingen, Germany) that was described by its manufacturers as a porous glass ceramic infiltrated by polymers. Because of this they are known as PICN64 (polymer infiltrated ceramics network).
These ceramics have 86% glass phase and 14% polymer, infiltrated at different pressures and temperatures, to obtain ceramics of different densities, in order to improve both their mechanical and optical qualities63,65.
Obtaining with it for the first time a restorative material with the same characteristics of enamel and dentin.
Subsequent to this launch, nano-ceramic blocks of composite resin reinforced with nano fillers have been launched on the dental market, such as Lava Ultimate (3M ESPE)66, or nano-hybrid fillers such as Cerasmart (GC Europe), Brava Block (FGM, Joinville. Santa Catarina, Brazil), among others.
Mechanical and optical properties
They have a flexural resistance of up to 160 MPa, this is half of what lithium disilicates reach, but three times more than feldspathic ones have. Similarly when compared to the flexural strength of polymers that is around 130 MPa, it can be seen that this value increases in the PICN.
This is achieved because the pores of the ceramic are filled, at the time of infiltration, by the polymer, and when a force tries to deform the body, it reacts by concentrating the stress in the polymeric zone, much more elastic, than the ceramic phase and In this way it is able to dissipate the forces that could break it. This is the same reason why they have an elastic modulus of 16-28.1 GPa that is much larger than the other ceramics and composites64.
It is very well known that feldspathic and disilicates do not withstand deformation beyond 0.1 to 0.2% before fracturing, therefore they are fragile, but PICNs are capable of withstanding deformation stresses up to 4.1 % before breaking. Which would improve the clinical life of the restorations because if it is able to withstand high deformations it is very possible that it supports very well the masticatory loads.
It is also interesting to note that the elastic dentin module is between 16 and 20.3 GPa, very similar to the 16-28.1 of the PICN, which would favor the presence of a more uniform stress between these two substrates when they are joined by means of an adhesive agent, when supporting the masticatory loads.
As for its optical properties, it is true that manufacturers provide a large range of colors and glare, with layers of transparent and opaque resin that try to resemble dentin and enamel, until today, the PICN can not match the optical characteristics of natural teeth67.
Unlike the other ceramics, there is a loss of brightness in these over time.
Microstructure
These materials are manufactured at high temperatures and high pressures, which is why they reach high percentages of degrees of conversion (85%) which greatly improves their mechanical properties68 by following two steps: first a network of vitreous and porous ceramic is produced and conditioned by a bonding agent. Second, the vitreous phase of the ceramic is replaced and at the same time infiltrated with a polymer by capillary action64,65.
To produce a PICN manufacturers manipulate the size of the ceramic particle, using different cooking temperatures, then it is chemically treated with a bonding agent usually a silane, and then fill its pores with UDMA, TEDMA and other methacrylate monomers, which they will be subjected to heat so that they polymerize inside her skeleton64.
This allows the formation of two distinct phases: the one ceramic and the other polymeric, which replaces the fragile vitreous phase of the other ceramics.
This new element thus formed will then have a reduced fragility and stiffness along with an improved fracture resistance and adequate hardness to be more easily worked in the CAD CAM.
The potential for wear or abrasion of PICN with antagonistic natural teeth is much less than that of vitreous ceramics.
Clinical uses
In spite of its limitations in its long-term optical properties, with these new materials, unit crowns, inlays, inlays, onlays, overlays, crowns on implants and adhesive restorations are being made with the technique of minimum preparation or minimum wear in areas of anterior teeth to replace a single tooth69.
However, more long-term clinical studies are needed to compare the PICN versus other dental ceramics.
Processing
Parts can be obtained through CAD CAM, followed by polymerization, which can be high temperature and high pressure (HT-HP).
Discussion
Since its appearance in 1960, dental ceramics have undergone an undoubted evolution and change of both their mechanical and optical properties, to resemble a natural tooth in its color, texture and resistance to wear and masticatory forces.
The first porcelains were feldspathic which, when obtained from the fusion of feldspar by means of a heat treatment process at high temperatures (800 to 12000C), are capable of forming a glassy element, which contains crystalline leucite nuclei2. These two phases make these porcelains have excellent optical characteristics, but poor mechanical conditions, therefore they are incapable of resisting occlusion forces and require mechanical support to survive in the mouth. They are the ones used to make crowns and bridges made of metal-porcelain.
Nowadays, thanks to the remarkable advances of dental adhesives, these porcelains can be used in the incisors and canines, when it comes to making aesthetic veneers, with the condition that they are attached to dental enamel17.
They do not have good results when they are supported by dentin.
The leucites have crystalline nuclei larger than the previous porcelains and have a vitreous phase in a smaller proportion which makes them more resistant and with good mechanical properties. They are very useful for veneers on anterior teeth, in the same way they must always be adhered to enamel. Like feldspats, they are used in the so-called "contact lens veneers". But they still have high rates of failure or fracture when crowns and dental bridges are made.
Vitreous lithium disilicate ceramics already have much longer and larger disilicate crystals inside them that are surrounded by a vitreous matrix31. But this structure thus formed is the result of a process called ceramization which allows manufacturers to modify and improve their mechanical resistance properties by varying the cooking temperature and thereby produce a ceramic material almost without micropores.
With all these conditions, lithium disilicates are able to resist and tolerate chewing forces of up to 400 Mpa. With which you could already make total crowns without metal in areas of premolars and bridges of up to three units in previous ones with very good long-term results40.
Finally, crystalline ceramics such as zirconias do not have a vitreous matrix, but they are only made up of the almost perfect union of zirconium crystals, that also has the unique characteristic that when they are subjected to stress or an external stimulus that they try to damage them, they are transformed from their tetragonal phase to monoclinic52. This unique phenomenon in ceramic materials is accompanied by an increase in volume by 5%. What compresses the advance of any microfissure that has formed internally, preventing its path, making the fracture of the material more difficult.
All these characteristics make it a very hard, and highly resistant body.
For this reason, large bridges can now be made in posterior areas, individual crowns, and implant structures, including implants. But it makes cementation very difficult.
The correct technique to adhere a piece of Y-TZP to the tooth involves the use of a tribochemical sandblasting, followed by silanes and adhesives based on acidic phosphate monomers. (10 MDP)58.
Conclusions
Dental ceramics have gradually overcome their limitations to the point of becoming highly sought after restorative elements by dentists, patients, and dental technicians.
Today there are several types of ceramics, each with different characteristics which allow the dentist to rehabilitate teeth with excellent naturalness.
There are long-term clinical studies of many of these ceramics, in other countries, however in our country we do not have data to confirm or discard these results, it would be very useful to develop research in our environment.
Bibliografía
- Rosenblum MA, Schulman A. A Review of All-Ceramic Restorations. The Journal of the American Dental Association. 1997;128(3):297-307.
- Cesar P. Cerâmicas odontológicas. Acedido em. 2011;13(05).
- Shenoy A, Shenoy N. Dental ceramics: An update. Journal of conservative dentistry: JCD. 2010;13(4):195.
- Craig RG, Powers JM. Materiais dentários restauradores: Santos; 2004.
- Gomes E, Assunção W, Rocha E, Santos P. Ceramic in dentistry: current situation. Cerâmica. 2008;54(331):319-25.
- Gracis S, Thompson VP, Ferencz JL, Silva NR, Bonfante EA. A new classification system for all-ceramic and ceramic-like restorative materials. International Journal of prosthodontics. 2015;28(3).
- Denry IL. Recent Advances in Ceramics for Dentistry. Critical Reviews in Oral Biology & Medicine. 1996;7(2):134-43.
- Al-Harthi AA, Aljoudi M, Almaliki M, El-Banna K. Laboratory Study of Micro-shear Bond Strength of Two Resin Cements to Leucite Ceramics using Different Ceramic Primers. The journal of contemporary dental practice. 2018;19(8):918-24.
- Stangel I, Nathanson D, Hsu C. Shear strength of the composite bond to etched porcelain. Journal of dental research. 1987;66(9):1460-5.
- Spohr AM, Sobrinho LC, Consani S, Sinhoreti MAC, Knowles JC. Influence of surface conditions and silane agent on the bond of resin to IPS Empress 2 ceramic. International Journal of Prosthodontics. 2003;16(3).
- Cesar PF, Yoshimura HN, Júnior WGM, Okada CY. Correlation between fracture toughness and leucite content in dental porcelains. Journal of dentistry. 2005;33(9):721-9.
- Morena R, Lockwood P, Fairhurst C. Fracture toughness of commercial dental porcelains. Dental Materials. 1986;2(2):58-62.
- Cattell MJ, Chadwick TC, Knowles JC, Clarke RL, Lynch E. Flexural strength optimisation of a leucite reinforced glass ceramic. Dental Materials. 2001;17(1):21-33.
- Denry IL, Mackert JR, Holloway JA, Rosenstiel SF. Effect of Cubic Leucite Stabilization on the Flexural Strength of Feldspathic Dental Porcelain. Journal of dental research. 1996;75(12):1928-35.
- Cattell MJ, Clarke RL, Lynch EJR. The transverse strength, reliability and microstructural features of four dental ceramics — Part I. Journal of Dentistry. 1997;25(5):399-407.
- Quinn J, Sundar V, Lloyd IK. Influence of microstructure and chemistry on the fracture toughness of dental ceramics. Dental Materials. 2003;19(7):603-11.
- Gresnigt MM, Cune MS, Schuitemaker J, van der Made SA, Meisberger EW, Magne P, et al. Performance of ceramic laminate veneers with immediate dentine sealing: An 11 year prospective clinical trial. Dental Materials. 2019;35(7):1042-52.
- Beier US, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. International Journal of Prosthodontics. 2012;25(1):79-85.
- Layton DM, Walton TR. The up to 21-year clinical outcome and survival of feldspathic porcelain veneers: accounting for clustering. International Journal of Prosthodontics. 2012;25(6).
- Ong JL, Farley DW, Norling BK. Quantification of leucite concentration using X-ray diffraction. Dental Materials. 2000;16(1):20-5.
- Mackert Jr J, Williams A. Microcracks in dental porcelain and their behavior during multiple firing. Journal of dental research. 1996;75(7):1484-90.
- Mackert Jr J, Rueggeberg E, Lockwood P, Evans A, Thompson W. Isothermal anneal effect on microcrack density around leucite particles in dental porcelain. Journal of dental research. 1994;73(6):1221-7.
- Mackert JR, Williams AL, Ergle JW, Russell CM. Water-enhanced crystallization of leucite in dental porcelain. Dental Materials. 2000;16(6):426-31.
- Morena R, Lockwood PE, Fairhurst CW. Fracture toughness of commercial dental porcelains. Dental Materials. 1986;2(2):58-62.
- Kon M, Kawano F, Asaoka K, Matsumoto N. Effect of Leucite Crystals on the Strength of Glassy Porcelain. Dental Materials Journal. 1994;13(2):138-47,269.
- Maunula H, Hjerppe J, Lassila LL, Närhi T. Optical Properties and Failure Load of Thin CAD/CAM Ceramic Veneers. The European journal of prosthodontics and restorative dentistry. 2017;25(2):86-92.
- Kelly JR, Benetti P. Ceramic materials in dentistry: historical evolution and current practice. Australian dental journal. 2011;56:84-96.
- Krämer N, Taschner M, Lohbauer U, Petschelt A, Frankenberger R. Totally bonded ceramic inlays and onlays after eight years. Journal of Adhesive Dentistry. 2008;10(4).
- Zarone F, Di Mauro MI, Ausiello P, Ruggiero G, Sorrentino R. Current status on lithium disilicate and zirconia: a narrative review. BMC Oral Health. 2019;19(1):134.
- Albakry M, Guazzato M, Swain MV. Influence of hot pressing on the microstructure and fracture toughness of two pressable dental glass–ceramics. Journal of Biomedical Materials Research Part B: Applied Biomaterials: An Official Journal of The Society for Biomaterials, The Japanese Society for Biomaterials, and The Australian Society for Biomaterials and the Korean Society for Biomaterials. 2004;71(1):99-107.
- Zarone F, Ferrari M, Mangano FG, Leone R, Sorrentino R. “Digitally oriented materials”: focus on lithium disilicate ceramics. International journal of dentistry. 2016;2016.
- Lien W, Roberts HW, Platt JA, Vandewalle KS, Hill TJ, Chu T-MG. Microstructural evolution and physical behavior of a lithium disilicate glass–ceramic. Dental materials. 2015;31(8):928-40.
- Belli R, Geinzer E, Muschweck A, Petschelt A, Lohbauer U. Mechanical fatigue degradation of ceramics versus resin composites for dental restorations. Dental Materials. 2014;30(4):424-32.
- Song X-F, Ren H-T, Yin L. Machinability of lithium disilicate glass ceramic in in vitro dental diamond bur adjusting process. Journal of the mechanical behavior of biomedical materials. 2016;53:78-92.
- Bühler-Zemp P, Völkel T. IPS e. max CAD Scientific documentation. Ivoclar Vivadent. 2005:1-16.
- Forster A, Ungvári K, Györgyey Á, Kukovecz Á, Turzó K, Nagy K. Human epithelial tissue culture study on restorative materials. Journal of dentistry. 2014;42(1):7-14.
- Höland W, Apel E, van‘t Hoen C, Rheinberger V. Studies of crystal phase formations in high-strength lithium disilicate glass–ceramics. Journal of Non-Crystalline Solids. 2006;352(38-39):4041-50.
- Denry I, Holloway J. Ceramics for dental applications: a review. Materials. 2010;3(1):351-68.
- Fasbinder DJ, Dennison JB, Heys D, Neiva G. A Clinical Evaluation of Chairside Lithium Disilicate CAD/CAM Crowns. The Journal of the American Dental Association. 2010;141:10S-4S.
- Gehrt M, Wolfart S, Rafai N, Reich S, Edelhoff D. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clinical Oral Investigations. 2013;17(1):275-84.
- Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999;20(1):1-25.
- Christel P, Meunier A, Dorlot JM, Crolet JM, Witvoet J, Sedel L, et al. Biomechanical compatibility and design of ceramic implants for orthopedic surgery. Annals of the New York Academy of Sciences. 1988;523(1):234-56.
- Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. Current status of zirconia restoration. Journal of prosthodontic research. 2013;57(4):236-61.
- Kelly JR, Denry I. Stabilized zirconia as a structural ceramic: an overview. Dental materials. 2008;24(3):289-98.
- Denry I, Kelly JR. State of the art of zirconia for dental applications. Dental materials. 2008;24(3):299-307.
- Manicone PF, Iommetti PR, Raffaelli L. An overview of zirconia ceramics: basic properties and clinical applications. Journal of dentistry. 2007;35(11):819-26.
- Kern M, Thompson VP. Bonding to glass infiltrated alumina ceramic: Adhesive methods and their durability. The Journal of Prosthetic Dentistry. 1995;73(3):240-9.
- Kirmali O, Kustarci A, Kapdan A, Er K. Efficacy of surface roughness and bond strength of Y-TZP zirconia after various pre-treatments. Photomedicine and laser surgery. 2015;33(1):15-21.
- De Mello CC, Bitencourt SB, dos Santos DM, Pesqueira AA, Pellizzer EP, Goiato MC. The Effect of Surface Treatment on Shear Bond Strength between Y-TZP and Veneer Ceramic: A Systematic Review and Meta-Analysis. Journal of Prosthodontics. 2018;27(7):624-35.
- Garvie R, Hannink R, Pascoe R. Ceramic steel? Nature. 1975;258(5537):703.
- Kim JE, Kim JH, Shim JS, Roh BD, Shin Y. Effect of Surface Treatment on Shear Bond Strength between Resin Cement and Ce-TZP/Al2O3. Biomed Res Int. 2016;2016:7576942.
- Guazzato M, Albakry M, Ringer SP, Swain MV. Strength, fracture toughness and microstructure of a selection of all-ceramic materials. Part II. Zirconia-based dental ceramics. Dental Materials. 2004;20(5):449-56.
- 53. Miranda RBP, Miranda WGJ, Lazar DRR, Ussui V, Marchi J, Cesar PF. Effect of titania content and biomimetic coating on the mechanical properties of the Y-TZP/TiO2 composite. Dent Mater. 2018;34(2):238-45.
- Baldissara P, Llukacej A, Ciocca L, Valandro FL, Scotti R. Translucency of zirconia copings made with different CAD/CAM systems. The Journal of prosthetic dentistry. 2010;104(1):6-12.
- Le M, Larsson C, Papia E. Bond strength between MDP-based cement and translucent zirconia. Dent Mater J. 2019;38(3):480-9.
- Araujo AMM, Januario A, Moura DMD, Tribst JPM, Ozcan M, Souza ROA. Can the Application of Multi-Mode Adhesive be a Substitute to Silicatized/Silanized Y-TZP Ceramics? Braz Dent J. 2018;29(3):275-81.
- Dal Piva AMO, Carvalho RLA, Lima AL, Bottino MA, Melo RM, Valandro LF. Silica coating followed by heat-treatment of MDP-primer for resin bond stability to yttria-stabilized zirconia polycrystals. J Biomed Mater Res B Appl Biomater. 2019;107(1):104-11.
- Melo R, Souza R, Dursun E, Monteiro E, Valandro L, Bottino M. Surface treatments of zirconia to enhance bonding durability. Operative dentistry. 2015;40(6):636-43.
- Yue X, Hou X, Gao J, Bao P, Shen J. Effects of MDP-based primers on shear bond strength between resin cement and zirconia. Exp Ther Med. 2019;17(5):3564-72.
- Ahn JS, Yi YA, Lee Y, Seo DG. Shear Bond Strength of MDP-Containing Self-Adhesive Resin Cement and Y-TZP Ceramics: Effect of Phosphate Monomer-Containing Primers. Biomed Res Int. 2015;2015:389234.
- Yang L, Chen B, Xie H, Chen Y, Chen Y, Chen C. Durability of Resin Bonding to Zirconia Using Products Containing 10-Methacryloyloxydecyl Dihydrogen Phosphate. J Adhes Dent. 2018;20(4):279-87.
- Treccani L, Klein TY, Meder F, Pardun K, Rezwan K. Functionalized ceramics for biomedical, biotechnological and environmental applications. Acta biomaterialia. 2013;9(7):7115-50.
- He L-H, Swain M. A novel polymer infiltrated ceramic dental material. Dental Materials. 2011;27(6):527-34.
- Coldea A, Swain MV, Thiel N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dental Materials. 2013;29(4):419-26.
- Della Bona A, Corazza PH, Zhang Y. Characterization of a polymer-infiltrated ceramic-network material. Dental Materials. 2014;30(5):564-9.
- Lawson NC, Bansal R, Burgess JO. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dental Materials. 2016;32(11):e275-e83.
- Eldafrawy M, Nguyen JF, Mainjot AK, Sadoun MJ. A Functionally Graded PICN Material for Biomimetic CAD-CAM Blocks. Journal of dental research. 2018;97(12):1324-30.
- Nguyen J-F, Migonney V, Ruse ND, Sadoun M. Resin composite blocks via high-pressure high-temperature polymerization. Dental Materials. 2012;28(5):529-34.
- Mainjot AK, Dupont NM, Oudkerk JC, Dewael TY, Sadoun MJ. From Artisanal to CAD-CAM Blocks: State of the Art of Indirect Composites. Journal of dental research. 2016;95(5):487-95.

Reconocimiento-NoComercial-CompartirIgual
CC BY-NC-SA
Esta licencia permite a otros entremezclar, ajustar y construir a partir de su obra con fines no comerciales, siempre y cuando le reconozcan la autorÍa y sus nuevas creaciones estÉn bajo una licencia con los mismos tÉrminos.