Plasma rico en fibrina (PRF) y placa de titanio en el tratamiento exitoso de un defecto óseo asociado a osteonecrosis causado por bisfosonatos: reporte de caso
Successful fibrin-rich plasma (frp) therapy and titanium plate for treating bone defect caused by bisphosphonates related osteonecrosis: a case report
Terapia bem sucedida com plasma rico em fibrina (frp) e placa de titânio para o tratamento de defeitos ósseos causados por osteonecrose relacionada aos bifosfonatos: relato de caso
Ricardo Ramalho Vecchiatti1, Thaís Gimenez Miniello2
RECIBIDO: 18/12/2018 ACEPTADO: 29/03/2019 PUBLICADO: 01/12/2019
- Specialization Coordinator Courses in Implantodontics at Unig - Iguaçu University and the Brazilian Association of Regional Dentistry Nova Iguaçu – Rio de Janeiro, Brazil (maxilofacial@globomail.com; Vecchiatti RR).
- Stomatology Department, School of Dentistry, University of Sao Paulo, Sao Paulo, Brazil. (thaminiello@usp.br; Miniello TG).
CORRESPONDENCIA
Thaís Gimenez Miniello
Stomatology Department, School of Dentistry,
University of Sao Paulo, Sao Paulo, Brazil. Av. Prof. Lineu Prestes, 2227 - Cidade Universitária - Butantã, CEP: 05508-000. São Paulo, SP, Brazil. Tel.: +55 11 3091-7901.
thaminiello@usp.br
RESUMEN
La osteonecrosis de la mandíbula asociada a bisfosfonatos (BRONJ) es una afección progresiva que aún no tiene consenso sobre su tratamiento ideal. La terapia con plasma rico en fibrina (PRF) ha demostrado ser efectiva en BRONJ. El presente caso relata el tratamiento de un paciente masculino de 76 años que asistió quejándose de dolor en la boca durante 8 meses. Su historial médico reportó metástasis de mieloma múltiple y uso de bisfosfonatos, que había dejado de tomar tres meses antes. En la mandíbula posterior izquierda, la evaluación clínica intraoral presentó supuración y exposición ósea de aproximadamente 4 cm; en la radiografía panorámica se identificó una imagen radiotransparente y desorganización de trabéculas óseas; en la tomografía computarizada fue evidente cierta destrucción de la cortical lingual y bucal, que sugirió secuestro óseo. El diagnóstico fue osteonecrosis asociada a bisfosfonatos. El tratamiento consistió en extraer el hueso necrótico y llenar el defecto con PRF obtenido de la sangre del paciente. Se consiguió el cierre completo de la herida. Después de 2 meses, el paciente volvió a quejarse de dolor, una radiografía panorámica mostró una línea radiolúcida de discontinuidad, sugestiva de fractura mandibular en la zona tratada previamente. Se realizó una segunda cirugía con acceso extraoral ya que la mucosa oral se encontraba completamente sana. Se extrajo el hueso necrótico y se colocaron placas de titanio. Después de 3 meses de seguimiento, hubo signos de consolidación ósea y ausencia de dolor; el paciente pudo comer adecuadamente y su calidad de vida mejoró.
Palabras clave: Osteonecrosis de la mandíbula; oteonecrosis asociada a bisfosfonatos; ácido zoledrónico; plasma rico en fibrina.
ABSTRACT
Bisphosphonate related osteonecrosis of the jaw (BRONJ) is a progressive condition that still has no consensus about its ideal treatment. Fibrin-rich plasma (FRP) therapy shows effectiveness on BRONJ’s treatment by clinicians. A 76-year-old male patient attended for our evaluation complaining of pain in his mouth for 8 months. The medical history showed multiple myeloma metastasis and the use of bisphosphonate (BP) for metastasis control. On intraoral clinical evaluation, suppuration and exposed bone was evident on posterior left mandible measuring approximately 4 centimeters. On panoramic radiograph, we observed a radiolucent image and an area of osseous trabeculae disorganization on left mandible. Computed Tomography (CT) image showed some destruction of lingual and buccal cortical, suggestive of bone sequestration. The treatment was to remove all necrotic bone and fill the defect with FRP from the patient's own blood. Sutures were placed to provide wound primary closure and after 2 months without evidence of exposed bone, the patient came complaining with pain again. After a panoramic radiograph, it was clearly observed a radiolucent image with an image of a jaw discontinuity line, suggestive of mandible fracture in the same side treated before. New surgery was performed and as the intraoral mucosa was perfectly healthy, an extraoral access was made. All the necrotic bone was removed and titanium plates were placed. After 3 months following up, there were signs of bone consolidation and no pain complaint by patient. The patient was able to eating properly and had his quality of life improved.
Keywords: Osteonecrosis of the jaw; bisphosphonate-associated osteonecrosis; zoledronic acid; fibrin-rich plasma.
RESUMO
A osteonecrose da mandíbula associada aos bisfosfonatos (BRONJ) é uma condição progressiva que ainda não tem consenso sobre seu tratamento ideal. A terapia de Plasma Rico em Fibrina (PRF) tem demostrado ser eficaz no BRONJ. O presente caso relata o tratamento de um paciente do sexo masculino, 76 anos, que se apresentou com manifestação de dor na boca por 8 meses. Seu histórico médico relatou metástase de mieloma múltiplo e uso de bisfosfonatos, que ele havia parado de tomar três meses antes. Na mandíbula posterior esquerda, a avaliação clínica intraoral apresentou supuração e exposição óssea de aproximadamente 4 cm; na radiografia panorâmica, foi identificada uma imagem radiolúcida e desorganização das trabéculas ósseas; Na tomografia computadorizada, foi evidente alguma destruição do córtex lingual e bucal, o que sugeria sequestro ósseo. O diagnóstico foi oseonecrose associada a bisfosfonatos. O tratamento consistiu na extração do osso necrótico e preenchimento do defeito com PRF obtido do sangue do paciente. Foi alcançado o fechamento completo da lesão. No entanto, após 2 meses, o paciente apresentou novamente dor, uma radiografia panorâmica mostrou uma linha radiolúcida de descontinuidade, sugestiva de fratura mandibular na área previamente tratada. Uma segunda cirurgia foi realizada com acesso extra-oral, pois a mucosa oral estava completamente saudável. O osso necrótico foi removido e as placas de titânio foram colocadas. Após 3 meses de acompanhamento, houve sinais de consolidação óssea e ausência de dor; o paciente que poderia comer adequadamente e sua qualidade de vida melhorou.
Palavras-chave: Osteonecrose da mandíbula; osteonecrose associada a bisfosfonato; ácido zoledrónico; plasma rico em fibrina.
INTRODUCTION
The term antiresorptive agent-related osteonecrosis of the jaw (ARONJ) have been used for designate all bone necrosis that are caused by those medications, like bisphosphonates (BPs), denosumab and monoclonal antibody against receptor activator of NFκB ligand (RANKL). Some bone necrosis can occur using antiangiogenic therapy such as angiostatin, 4-platelet factor, endostatins and thalidomide or long-term systemic corticosteroid. BPs are drugs considered as antiresorptive agents used to treat patients with osteoporosis, metastatic bone cancer, or with some bone pathology with bone loss due to the increased bone resorption. Bisphosphonate related osteonecrosis of the jaw (BRONJ) are bone exposures on the maxillofacial region that does not heal after 8 week in patients with no previous craniofacial region irradiation, Marx et al., 20051.
Marx RE, 20032, reported for the first time on the exposure of the jaw and jaw bones of patients receiving bisphosphonates and subsequently, several authors reported additional cases. The prevalence is considered quite low and ranges between 0.1% and 0.21% for patients who take these drugs orally with longer than 4 years of use and between 0,7% and 6.7% for under intravenous (IV) treatment with zolendronic acid (ZA), Ruggiero et al., 20143. Mostly BRONJ are cause by some manipulation on bone or soft tissues in oral cavity (oral extractions or dental implant placement), but it can occur by spontaneously, Miniello et al., 20154. It depends on several factors such as therapeutic indication, medication administration route, dose, time of use, among others, Ruggiero et al., 20143.
Despite these low percentages, its management is always an enigma and in some cases, non resolutive therapeutic choices can affect patient's quality of life. Many points about BRONJs remain obscure and treatment still don´t has, until now, a consensus about an ideal or more resolutive. Most publications advice regarding prevention and management of this condition, which is not yet well established, Marx, 20032; Marx et al., 20051; Ruggiero et al., 20043. Some care for prevention include routine oral hygiene to reduce caries risk and periodontal disease, regular visits to dentist for reevaluation and clinical healthy preservation, Tong et al., 20105.
Treatments with the use of antibiotics (ATB) and hygiene with 0.12% cloredixidine gluconate are considered conservative, however, are more effective when combined with others treatments like bone debridement and/or resections surgery, considered invasive, Miniello et al., 20196. Some others treatments have been related as PENTO (pentoxifylline and tocopherol) protocol, platelet-rich plasma (PRP), fibrin-rich plasma (FRP), low-level laser therapy (LLLT), hyperbaric oxygenation (HBO), antimicrobial photodynamic therapy (aPDT), among others.
A literature review in PubMed (articles in English ranging from 1983 to 2017) selected and analyzed about BRONJ and their treatments. Protocol with PENTO associated with ATB did not showed good results (only 17% of success) in healing of BRONJ. HBO had contrasting results with varying success rates between 25% and 90%, depending on the year of publication of the study analyzed. LLLT was presented as a more efficient approach when combined with ATB and bone debridement. The most effective was PRP, succeeding in over 80% of cases. Even so, surgery is the treatment option more adopted for BRONJ, Schubert et al., 20127. A varying success rate among cases reported in literature, average treatment success with conservative surgery and extensive surgery are 53% and 67%, respectively. Therefore, the study concluded that these are challenging diseases with no specific treatment, Ribeiro et al., 20188.
The purpose of this paper is to relate a case about BRONJ treatment in a myeloma multiple patient in use of ZA that attended for our evaluation.
Case Report
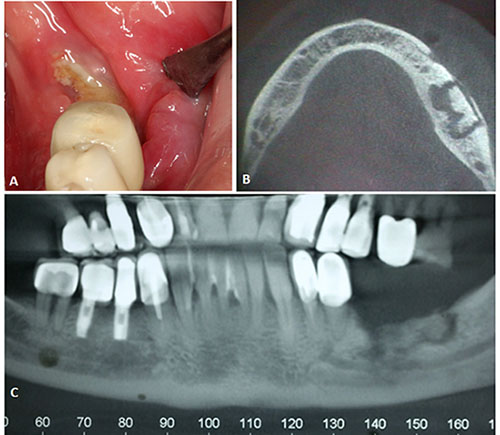
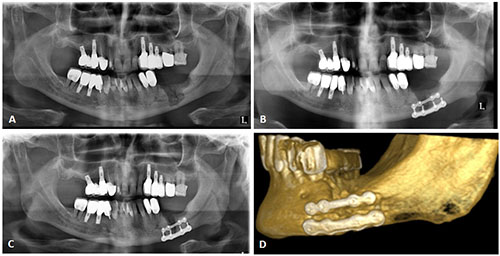
A 76-year-old male patient attended for our evaluation complaining of pain in his mouth after 8 months having consulted with several professionals. The medical history showed multiple myeloma metastasis and the use of BP, more specifically the ZA for metastasis control. On intraoral clinical evaluation, suppuration and exposed bone was evident on posterior left mandible measuring approximately 4 centimeters. On panoramic radiograph, we observed a radiolucent image and an area of osseous trabeculae disorganization on left mandible (figure 1).
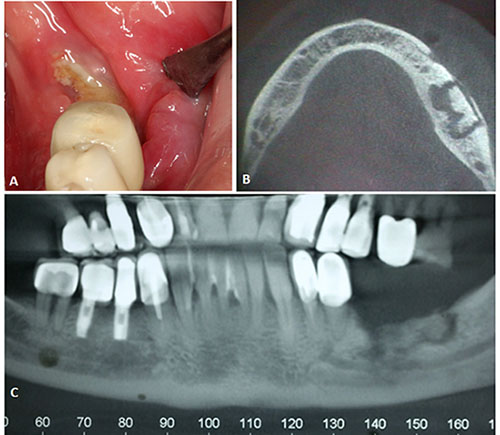
Figure 1. Initial clinical and radiographic aspects, A. Intraoral clinical evaluation: suppuration and exposed bone on posterior left mandible. B. Computed Tomography (CT) image showed some destruction of buccal cortical, suggestive of bone sequestration. C. Panoramic radiograph showed a radiolucent image and an area of osseous trabeculae disorganization.
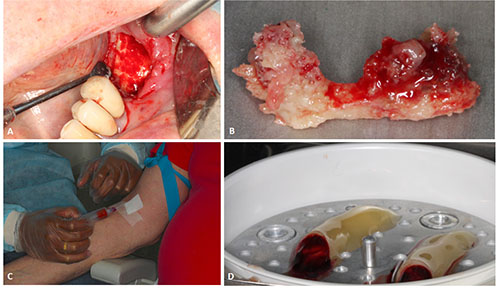
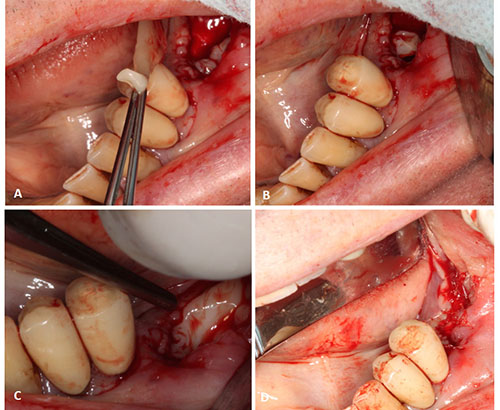
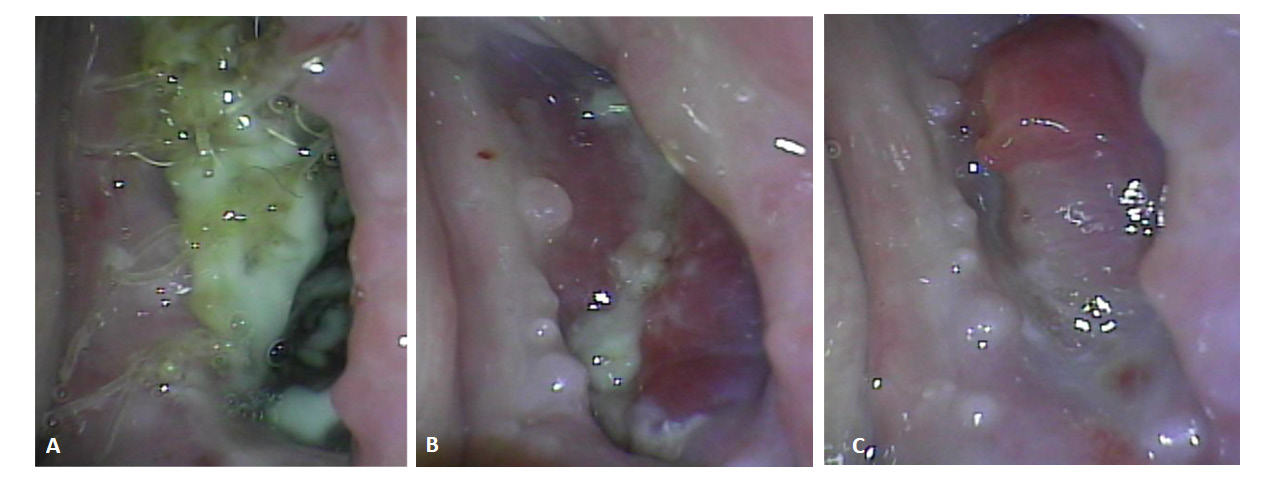
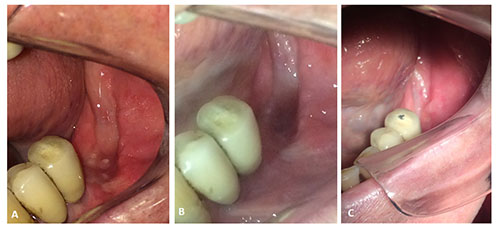
Computed Tomography (CT) image showed some destruction of lingual and buccal cortical, suggestive of bone sequestration (figure 1). Based on clinical and imaging features, treatment consisted on remove all necrotic bone and fill the defect with FRP from the patient's own blood. Sutures were placed to provide wound primary closure (figures 2 and 3). Intra oral soft tissue showed signs of favorable healing (figure 4).
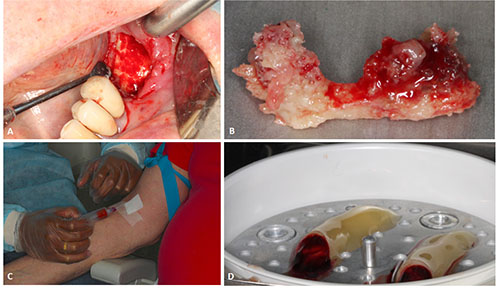
Figure 2. Treatment with FRP, A.Incision and access to necrotic tissue. B. Necrotic surgical specimen removed. C. Patient's own blood collection. D. Blood was adjusted for centrifugation 12 minutes at 3000 revolutions per minute and the FRP was obtained immediately after the procedure.
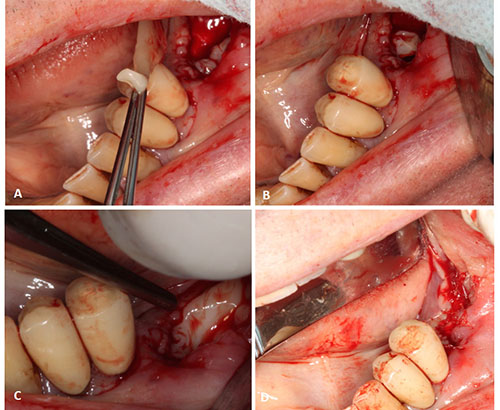
Figure 3. Placement and adjustment of the FRP in surgical defect. D. Sutures placed to provide wound primary closure
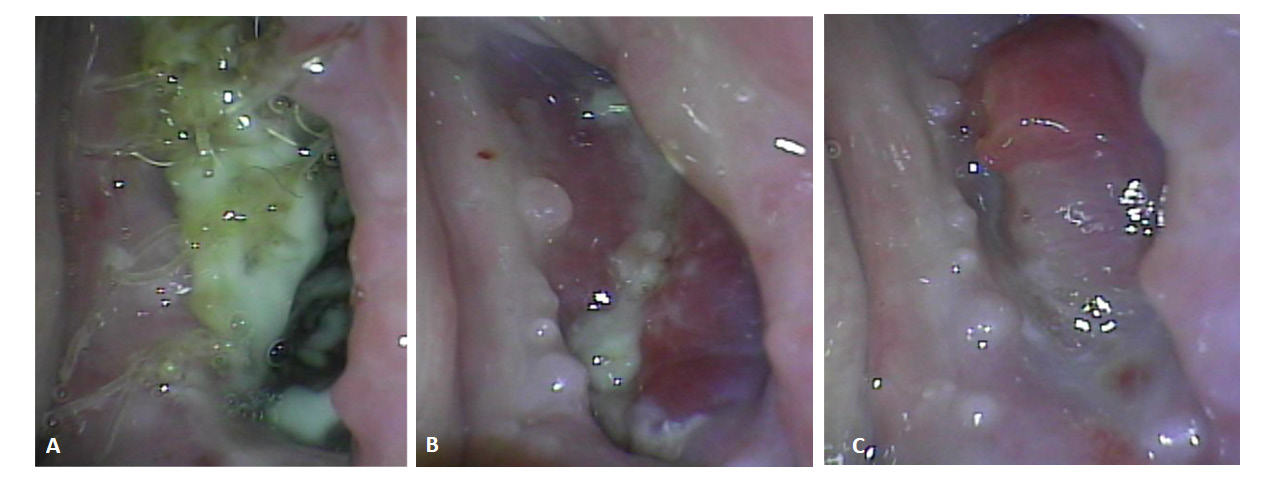
Figure 4. Intra oral soft tissue showed signs of favorable healing, A. Seven days postoperatively. B. Fourteen days postoperatively. C. Twenty one days postoperatively
After 2 months without evidence of exposed bone, the patient came complaining with pain again. After a panoramic radiograph, it was clearly observed a radiolucent image with an image of a jaw discontinuity line, suggestive of mandible fracture in the same side treated before. Therefore, under general anesthesia, new surgery was performed, however, as the intraoral mucosa was perfectly healthy, it was an extraoral access in this time. All the necrotic bone was removed and titanium plates were placed for favoring bone consolidation (figure 5).
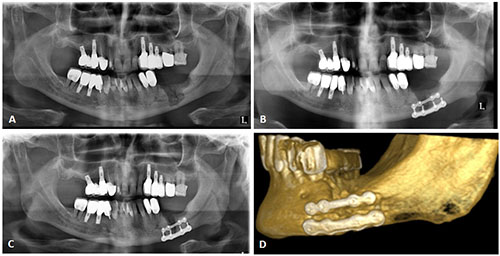
Figure 5. Panoramic radiograph and CT after 2 months without intraoral exposed necrotic bone, Panoramic radiograph showing a radiolucent image with an image of a jaw discontinuity line, suggestive of mandible fracture. B. After extraoral acess the necrotic bone was removed and titanium plates were placed. C/D. Panoramic radiograph and CT three months postoperatively with signs of bone consolidation.
After 3 months following up, there were signs of bone consolidation and no pain complaint by patient. The intraoral mucosa remained intact and no bone exposure was observed until 7 months following up. The patient was able to eating properly and had his quality of life improved (figure 6).
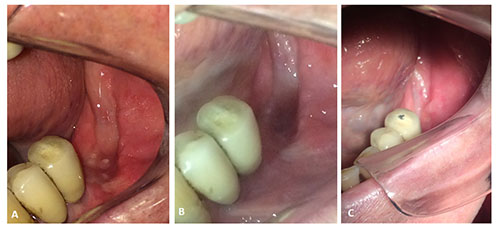
Figure 6. Final extraoral aspect, A. Three months post treatment. B. Four months post treatment. C. Seven months post treatment. Healed and closed mucosa without bone exposures.
Discussion
Current studies found in literature indicate BRONJ lesions treatment with PRP and platelet-rich fibrin (PRF). Very few studies report the use of FRP. With this case report we have demonstrated the possibility that this treatment can be effective and promising. Valente et al., 20199, performed a retrospective study that analyzed records from patients with documented ARONJ treated in their unit. They analyzed data between June 2016 and January 2017of 15 patients, with mean age of 64 years. About 60% of the sample used zolendronate or denosumab and causative factors like dental extraction trigger rate of 33.3%, a spontaneous ARONJ 40%. Treatment success rate of 73.3%, but the authors report that the surgical treatment had to be repeated more than once. Of 14 cases that were treated with PRF following bone debridement led to the resolution of 11 patients (78,6%). Failure in this study rate of 26.6%, so, they concluded that PRF showed potential benefits in the in ARONJ resolution, but make it clear that this treatment has to be investigate in future studies.
Until now we didn't find many studies about FRP and osteonecrosis. Another preventive study with PRF was authored by of Asaka et al. 201710, that had an objective to evaluate the effectiveness of PRF as a healing accelerating agent in patients undergoing oral BP therapy (average of 32 months of use) and requiring dental extractions. They analyzed 102 patients divided into a PRF group and control group. There were no intraoperative complications and none of the patients had onset BRONJ. Delayed recovery was observed in 9 of 73 control patients (12%) and this was significantly higher in the control group than in the PRF group. The authors concluded that early epithelialization has been confirmed in all patients and that PRF may reduce the risk of delayed recovery in patients undergoing oral BP therapy and play a key role in preventing BRONJ.
Much has also been said about the role of leukocyte-rich and platelet-rich fibrin (L-PRF) in the treatment of BRONJ. Given the controversy and current lack of consensus regarding BRONJ therapy in patients, new techniques have been developed including the use of L-PRF. The purpose of the review by Cano-Durán et al. 201711, was to evaluate whether L-PRF would be really effective in BRONJ. The results showed that the use of L-PRF for the treatment of BRONJ is really effective, especially when performed with simultaneous application of L-PRF and morphogenetic protein-2 (BMP-2). Therefore, the authors concluded that the current literature demonstrates the efficacy of L-PRF use in osteonecrosis, and that can be considered a real alternative in the treatment of this disease. However, more clinical studies are needed to really evaluate this new therapy and success depends on several factors, such as the previous existence of infection or the clinical stage the patient is in.
The analysis of our study can set the standard for the initiation of new studies that aim to seek the effectiveness in the treatment of BRONJ, since there is no fully effective one reported to date. According to current studies, platelet concentrates have been widely used in a variety of medical fields to promote soft and hard tissue regeneration by generating many growth factors and promoting wound healing; which is also found in the FRP, Babade et al., 201612.
Conclusion
In this particular case, as FRP initially helped complete healing of intraoral soft tissue, extraoral access was a more palatable option on second surgery for removal all affected bone tissue. However, even if the use of plates is not very common in patients using or who have already used BP, in this case it was the only option for a possible bone consolidation in the mandibular fracture region. Therefore, after 3 months by titanium plates placed, there were signs of bone consolidation. The patient was able to eating properly and had his quality of life improved, with no pan complaint or other complications.
Bibliografía
- Marx RE, Sawatari Y, Fortin M, et al. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg 2005;63:1567–1575.
- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: A growing epidemic. J Oral Maxillofac Surg 2003; 61:1115.
- Ruggiero SL, Dodson TB, Fantasia J, et al. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg 2014;72:1938–56.
- Miniello TG, Araújo JP, Lopes RN, Alves FA. Osteonecrosis related to once-yearly zoledronic acid treatment in an osteoporotic patient after dental implant. Braz Dent J. 2015 Jan-Feb;26(1):86-8. doi: 10.1590/0103-6440201300255.
- Tong CK, Ho ST, Wong SL. Osteonecrosis of the jaw after oral bisphosphonate for osteoporosis. Hong Kong Med J. 2010;16:145-8.
- Miniello TG, Araújo JP, Silva MLG, Paulo Kowalski L, Rocha AC, Jaguar GC, Abreu Alves F. Influence of bisphosphonates on clinical features of osteoradionecrosis of the maxilla and mandible. Oral Dis. 2019 Jul;25(5):1344-1351. doi: 10.1111/odi.13081.
- Schubert M, Klatte I, Linek W, Muller B, Doring K, Eckelt U, et al. The saxon bisphosphonate register - therapy and prevention of bisphosphonate-related osteonecrosis of the jaws. Oral Oncol. 2012;48:349-54.
- Ribeiro GH, Chrun ES, Dutra KL, Daniel FI, Grando LJ. Osteonecrosis of the jaws: a review and update in etiology and treatment. Braz J Otorhinolaryngol. 2018;84:102-8.
- Valente NA, Chatelain S, Alfonsi F, Mortellaro C, Barone A. Medication-Related Osteonecrosis of the Jaw: The Use of Leukocyte-Platelet-Rich Fibrin as an Adjunct in the Treatment. J Craniofac Surg. 2019 Jun;30(4):1095-1101. doi: 10.1097/SCS.0000000000005475.
- Asaka T, Ohga N, Yamazaki Y, Sato J, Satoh C, Kitagawa Y. Platelet-rich fibrina may reduce the risk of delayed recovery in tooth-extracted patients undergoing oral bisphosphonate therapy: a trial study. Clin Oral Investig. 2017 Sep;21(7):2165-2172. doi: 10.1007/s00784-016-2004-z.
- Cano-Durán JA, Peña-Cardelles JF, Ortega-Concepción D, Paredes-Rodríguez VM, García-Riart M, López-Quiles J. The role of Leucocyte-rich and platelet-rich fibrin (L-PRF) in the treatment of the medication-related osteonecrosis of the jaws (MRONJ). J Clin Exp Dent. 2017 Aug 1;9(8):e1051-e1059. doi: 10.4317/jced.54154.
- Badade PS, Mahale SA, Panjwani AA, Vaidya PD, Warang AD. Antimicrobial effect of platelet-rich plasma and platelet-rich fibrin. Indian J Dent Res. 2016 May-Jun;27(3):300-4. doi: 10.4103/0970-9290.186231.

Reconocimiento-NoComercial-CompartirIgual
CC BY-NC-SA
Esta licencia permite a otros entremezclar, ajustar y construir a partir de su obra con fines no comerciales, siempre y cuando le reconozcan la autorÍa y sus nuevas creaciones estÉn bajo una licencia con los mismos tÉrminos.