RESUMEN
En implantología oral, ha sido motivo de investigación y constante evolución la interfase implante-pilar, principalmente desde el punto de vista biomecánico y biológico. Objetivo: Valorar el espacio o “gap” en la interfase implante-pilar en implantes de conexión hexagonal interna y externa por medio de microscopía electrónica de barrido (MEB). Materiales y Métodos: Estudio in vitro en 24 implantes (Bionnovation®) divididos en dos grupos (n=12): conexión hexagonal interna y externa. Para el experimento, se atornillaron pilares rectos con 30N de torque. A su vez 6 implantes por grupo se sometieron a 500000 ciclos de carga dinámica; posteriormente, se evaluó por MEB el espacio de la interfase implante pilar en 3 puntos de todas las muestras, las medias de los resultados de cada espécimen se respaldaron en tablas de Excel y se analizaron en el programa BioEstat 5.3. Resultados: Mediante test T para muestras independientes, con una significancia del 95%, se encontró una diferencia muy significativa luego de la aplicación de la carga dinámica en los implantes de hexágono externo (p= 0.0002). En los implantes de hexágono interno también existió diferencia estadística (p= 0.03). Entre los implantes de hexágono externo e interno existieron diferencias muy significativas en la precisión del ajuste en la interfase implante pilar antes y después de la aplicación de las cargas dinámicas (p= <0.0001 y p= 0.0003 respectivamente). Conclusiones: Las cargas dinámicas aumentaron significativamente la discrepancia en la conexión implante-pilar de los implantes de hexágono externo e interno (p= < 0.05); adicionalmente, la distancia del “gap” fue mayor para los implantes de hexágono externo en contraste con los implantes de Hexágono Interno antes y después de la carga dinámica, siendo muy significativo (p= < 0.0003).
Palabras clave: Implantes dentales, diseño de implante dental-pilar; ajuste de prótesis; prótesis e implantes; filtración dental.
ABSTRACT
In oral implantology, the implant-pillar interface has been a subject of research and constant evolution, mainly from the biomechanical and biological point of view. Objective: To assess the gap in the implant-abutment interface in internal and external hexagonal connection implants by means of scanning electron microscopy (SEM). Materials and Methods: In vitro study in 24 implants (Bionnovation®) divided into two groups (n = 12): internal and external hexagonal connection. For the experiment, straight pillars with 30N of torque were screwed. In turn, 6 implants per group underwent 500,000 cycles of dynamic loading; Subsequently, the space of the pillar implant interface at 3 points of all samples was evaluated by MEB, the means of the results of each specimen were supported in Excel tables and analyzed in the BioEstat 5.3 program. Results: Using a T test for independent samples, with a significance of 95%, a very significant difference was found after the application of the dynamic load in the external hexagon implants (p = 0.0002). In the internal hexagon implants there was also a statistical difference (p = 0.03). Between the external and internal hexagon implants there were very significant differences in the accuracy of the adjustment in the abutment implant interface before and after the application of the dynamic loads (p = <0.0001 and p = 0.0003 respectively). Conclusions: Dynamic loads significantly increased the discrepancy in the implant-abutment connection of the external and internal hexagon implants (p = <0.05); additionally, the gap distance was greater for external hexagon implants in contrast to Internal Hexagon implants before and after dynamic loading, being very significant (p = <0.0003).
Keywords: Dental implants, dental implant - abutment design; prosthesis fitting; prostheses and implants; dental leakage.
RESUMO
Na implantologia oral, a interface implante-pilar tem sido objeto de pesquisa e evolução constante, principalmente do ponto de vista biomecânico e biológico. Objetivo: Avaliar o espaço ou “gap” na interface implante-pilar em implantes de conexão hexagonal interna e externa por meio de microscopia eletrônica de varredura (MEV). Materiais e Métodos: Estudo in vitro em 24 implantes (Bionnovation®) divididos em dois grupos (n = 12): conexão hexagonal interna e externa. Para o experimento, pilares retos com 30N de torque foram parafusados. Por sua vez, 6 implantes por grupo passaram por 500.000 ciclos de carregamento dinâmico; posteriormente, o espaço da interface do implante de pilar em 3 pontos de todas as amostras foi avaliado pelo MEV, as médias dos resultados de cada amostra foram suportadas em tabelas Excel e analisadas no programa BioEstat 5.3. Resultados: Usando um teste T para amostras independentes, com significância de 95%, foi encontrada uma diferença muito significativa após a aplicação da carga dinâmica nos implantes hexagonais externos (p = 0,0002). Nos implantes hexagonais internos também houve diferença estatística (p = 0,03). Entre os implantes hexágono externo e interno, houve diferenças muito significativas na precisão do ajuste na interface do implante de pilar antes e após a aplicação das cargas dinâmicas (p = <0,0001 ep = 0,0003, respectivamente). Conclusões: As cargas dinâmicas aumentaram significativamente a discrepância na conexão implante-pilar dos implantes hexágono externo e interno (p = <0,05); além disso, a distância do gap foi maior para os implantes hexagonais externos, em contraste com os implantes de hexágono interno antes e após o carregamento dinâmico, sendo muito significativa (p = <0,0003).
Palavras-chave: Implantes Dentários; Conexão Implante Dentário-pivô; Ajuste de Prótese; Próteses e Implantes; Filtração Dentária.
INTRODUCTION
The constant evolution of implants and prosthetic components has improved their biological and mechanical characteristics. However, it is still a great challenge to offer a prosthetic rehabilitation treatment that is durable and at the same time allows the maintenance of surrounding structures such as bone and mucosa; among the factors that influence this balance, one of the main factors is the type of prosthetic interface1.
Since the introduction of dental implants and their respective prosthetic attachments, their connection has been a reason for constant research and development, known as the implant-abutment interface comprising the base of the abutment and implant platform. This interface has had great relevance of study since there may be both biomechanical and biological adverse conditions that generate complications, among the biological complications there is bacterial accumulation, which manages to affect the peri-implant tissues, which in turn can generate bone loss and probably lead to implant failure1. Poor adjustment accuracy of the implant-abutment connection and the quality of the materials that make up these superstructures have been attributed as the most important causes of marginal mismatch2-4.
The first implants were developed by superimposing the abutment on an external hexagonal interface, however, clinical complications have been described that caused the loosening and / or breakage of the screws, implant fractures and prosthetic components. To reduce these faults, mechanical connections with internal adjustment (hexagonal, triangular, octagonal or conical) were developed. With the advent and the various options of prosthetic interfaces available for rehabilitation planning, greater knowledge about their biomechanical characteristics and longevity is required7.
One of the main challenges for the clinician-implantologist is to choose a system whose implant-prosthesis connection is the most appropriate for the treatment plan, taking into account the biomechanical characteristics of the dental implant system, its experience, personal preference and final costs for the patient. To contribute to the knowledge about the implant-abutment interface, the size of the gap was compared by means of Scanning Electron Microscopy between the internal and external hexagonal connections with straight prefabricated pillars without load and under dynamic load.
Materials and methods
In vitro study approved by the Sub Committee of Ethics and Research of the Central University. On 24 Bionnovation® (SP, Brazil) implants with internal connection (Ø 3.5 mm) and external connection (Ø 3.75 mm), straight prosthetic abutments with an adjustment torque of 30 N / cm were mounted. Two groups were formed (n = 12), with Internal Hexagon and External Hexagon implants. Each group was subdivided into 6 implants with dynamic loading (experimental group) and 6 implants without loading (control group). To apply the load, a force of 120 N at 2 Hz was used for 500,000 cycles equivalent to eight months of human masticatory function5.
A scanning electron microscope (TESCAN® MIRA 3, PA. USA) was used to observe the distance or Gap at the abutment implant interface at three different points of the platform (mesial, medial and distal), which were coded with the acronym (Gap1,2,3). The study was conducted as follows:
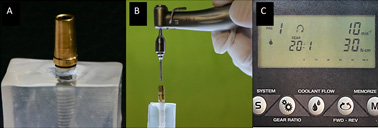
1. Implant placement and straight pillar fixation
For the experiment, 24 acrylic test tubes were made that received 24 Bionnovation® implants (SP, Brazil), placed at 90 ° with respect to the base (Figure 1A), coded according to the group they belonged (HE or HI). All straight prefabricated abutments of the same implant house (Bionnovation®) were bolted standardized and electromechanically with the Surgic pro® NSK implant motor (Japan) at 30 N / cm force (Figure 1B and 1C), both for implants Classic Bionnovation® external hexagon as for HI Bionnovation® internal hexagon (SP, Brazil).
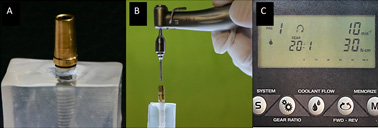
Figure 1. Screw fixation at 30N / cm2 (B); Torque standardization with Surgic Pro® engine (NSK, Japan).
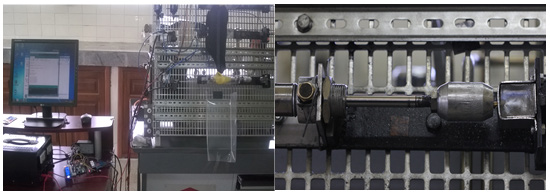
2.- Implants subjected to dynamic loading
Randomly, six test tubes from each group were placed in a magnetized receptacle for fixing in the dynamic load machine of the Faculty of Mechanical Engineering of the University of the Armed Forces - ESPE. Each group of implants (n= 6): 1A, external hexagon and 2C, internal hexagon, previously fixed in the test tubes were subjected to dynamic loads (5) at 120 N, 2 Hz for 500,000 cycles with an electro-pneumatic HERION LS system 2000. The working pressure, equivalent to 120 N, was regulated in the FRL unit of the HERION LS 2000 and corresponding to 3.69 bar and 500,000 cycles; which was used to calibrate on the gauge of the unit. The automatic control, for the 500,000 cycles, with a frequency of 2 Hz, (6) was established in the Arduino program, governed by an I 7 CPU, so that the system automatically stops once the established cycles have been reached (Figure 2). The samples were stored in airtight containers to avoid contamination, until observation by scanning electron microscope.
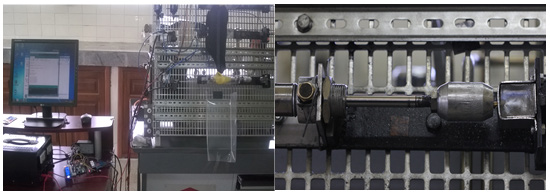
Figure 2. Samples subjected to dynamic loads for 500,000 cycles.
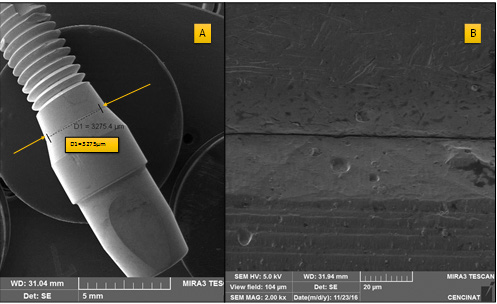
3. Scanning Electron Microscopy (MEB)
In both the groups under load and in the control, the adjustment of the connection at the implant-abutment interface was measured by scanning electron microscopy (SEM), without the need to section the specimen (Figure 3A). Previously, the 24 samples were immersed in 99% ethanol, subjected to ultrasound for one hour and under pressure with compressed air, to avoid impurities. Once the samples were dried, they were mounted on the microscopy stands and coated with double-face carbon tape (Electron Microscopy Sciences, PA, USA), and then introduced directly into the carousel of the scanning electron microscope TESCAN® MIRA 3 (PA, USES). The samples were observed with a voltage of 5 kV and with a working distance (1.2nm) of approximately 30 mm (Figure 3B)6.
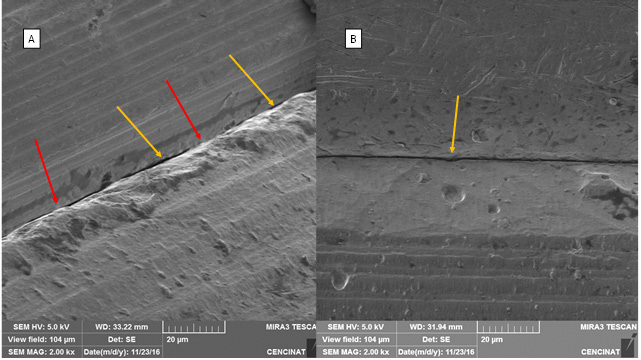
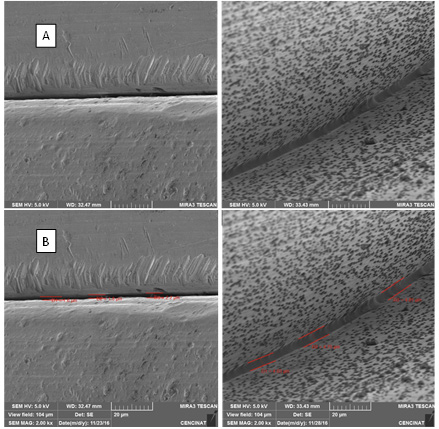
It was observed that the settlement of the abutment on the platform is not uniform, so three measurements were made per implant (Figure 4 A and B).
Figure 3. A: Sample assembly in MEB, scanning area. B: abutment implant interface.
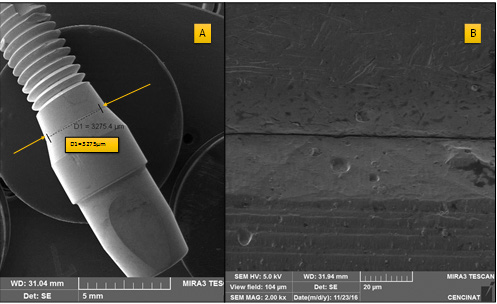
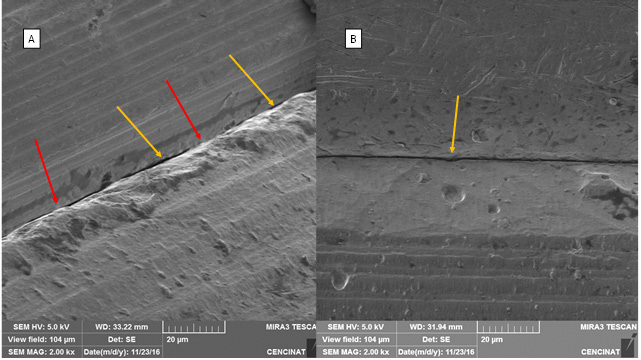
Figure 4. Irregular settlement of the abutment, vertical and horizontal discrepancy is observed. In yellow areas of lower settlement (A and B), in red areas of higher settlement
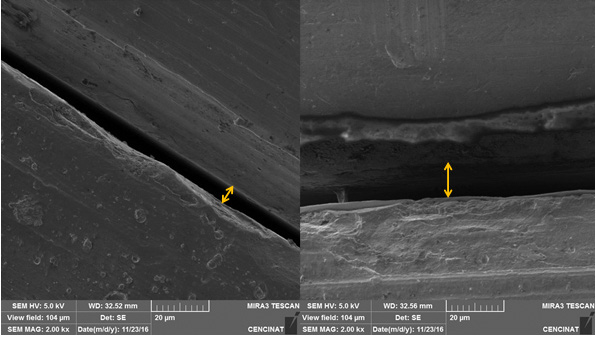
Once the micrographs were defined (Figure 5A), measurements were made in µ (figure 5B). In each sample three measurements were made and the average of each one was recorded, the results of each specimen subjected to dynamic loads and those of the control group were stored in excel sheets and subjected to descriptive and inferential statistical analysis.
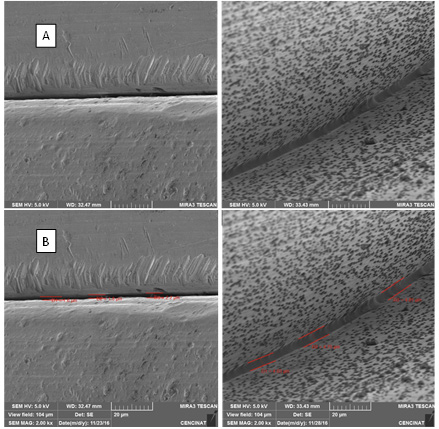
Figure 5. Micrographs of a section of the abutment implant interface (A). Measurements in µ (B).
It was observed that there was a great variation in the external hexagon group after dynamic loading (Figure 5)
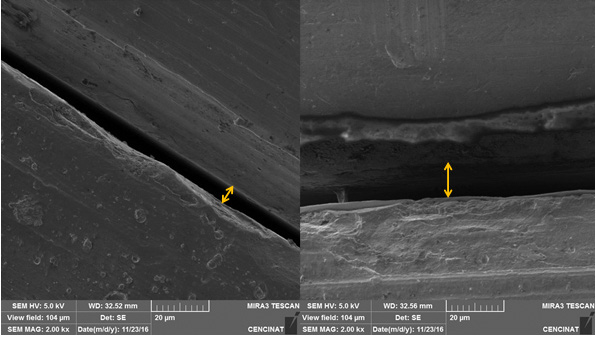
Figure 6. Greater discrepancy of the interface after the application of dynamic loads
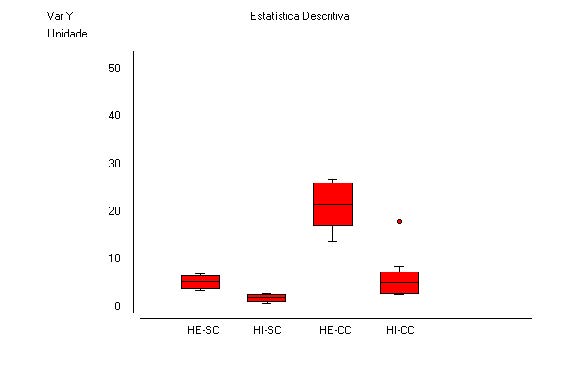
Figure 6. Greater discrepancy of the interface after the application of dynamic loads
Statistic analysis
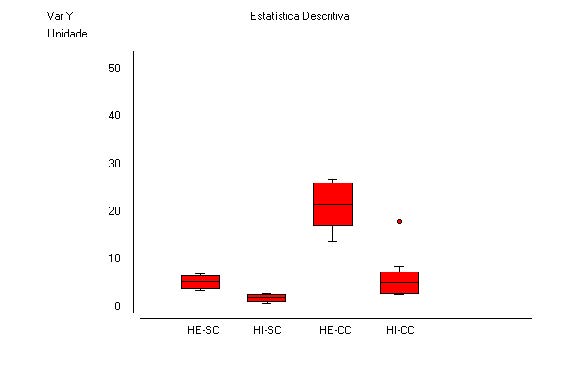
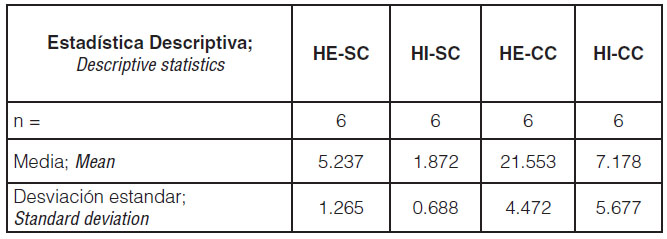
The quantitative data of the Gap were statistically analyzed using the BioEstat 5.3® software (Brazil). Lilliefors tests were performed to assess the difference with the normal curve. As the data met the requirements, descriptive statistics are presented as mean ± standard deviation (Table 1).
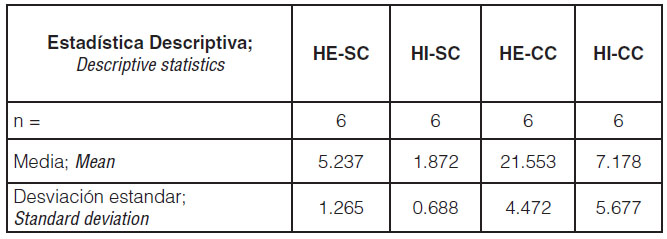
Picture 1. Means and standard deviation of each study group
Discussion
According to the results obtained in the present study, it was determined that the accuracy of the adjustment of the external connection between the prosthetic platform and the base of the abutment is lost to a greater degree than the internal connection against the dynamic loads, which is checked by a greater GAP discrepancy. But, it is relevant that both the external and internal hexagons have significant values after the number of cycles since it would correspond only to 8 months of use.
In the experimental group of external hexagon, the size of the pillar implant interface was larger, the values oscillating above 20 microns compared to the group of the internal hexagon less than 7 microns, these results agree with the mismatch of the external Hexagon described by Santos in 20137, who reported that the length of the external hexagon can influence the strength and stability of the implant interface connector. On the contrary, for Gil et al8, the longer external hexagon demonstrated better resistance to mechanical stress and better mechanical stability of dental implants.
The vertical marginal mismatch observed in the implant-pillar interface showed a marked deviation, ranging from 2 to 20 microns; If the shape of the abutment and the implant is circumferential, there may be variations of space in the general settlement, which indicates that it does not always maintain a uniform width from the base of the abutment9, as corroborated by Dias et al. in 2012.
It has been determined that the internal connection may have a better distribution of forces compared to external connections; as well as in its resistance to bending, due to the ability to distribute lateral forces homogeneously10,11; Although this criterion can be ratified with our research, it is important to consider that there was a statistically significant increase in the internal hexagon implant gap.
There is controversy in the literature about the range of tolerable values for the marginal discrepancy in the Gap of the studied interface12, especially in one-piece structures on multiple implants13. Binnon (1996), determined that the tolerance range in the marginal discrepancy vertically is up to 66 microns. In contrast to the current in vitro research, it would be accepted that the results obtained would be within the ranges determined by the author. The experimentation groups and control group were in ranges no greater than 25 microns. The evolution of the connection should establish lower ranges currently.
Existing studies analyzing the adjustment of the implant-abutment connection are scarce, the results being very heterogeneous, due in part to the fact that the methodology used differs considerably from one another10, probably depending on the type of connection and the brand of the implant.
The implant-pillar interface is an area susceptible to dimensional changes; characteristics of the abutment material, the type of load (axial or lateral), the force with which it is subjected; They can generate differences in results. The type of dynamic load used in the present investigation had the same parameters with the study of Costa Alves, C et al, 20166 with 500,000 cycles and 120 N force at 2 Hz, which represent 8 months of masticatory function as determines the ISO-2007 standard15. In vitro clinical studies have shown that 30.7% to 49% of fixation screws are lost in externally connected implants16, with values equal to the applied load.
The size of the interface was evaluated according to Kano et al in 200717, who makes a classification of the mismatch in the implant-pillar interface and suggests taking the measurements in 8 locations. As a limitation in the present investigation, this number of measurements could not be performed, 3 measurements were made per implant and an average of each sample was obtained (GAP: mesial, medial and distal). However, studies suggest that reliable results are obtained when several measurements are not taken along the margin, as mentioned by Groten et al. in the year 200018.
On the other hand, one of the drawbacks of this investigation was that although the photographs were taken at the same time, by the same operator and in the same microscope, some of them were not 100% clear and it was difficult to assess the size of the interface. In some cases the difference in size was atypical, which can generate errors in the analysis of results, determining a variation of the results, by the oscillation of the values depending on the angle of observation; Kano (2007), presented the same drawbacks17.
There is a long and incomparable casuistic significance in the type of external connection versus the evolutionary internal connections. This study, tried to strengthen and ratify criteria with serious investigations that have contributed to the sufficient information, it is evident that in the rehabilitation of multiple implants where the prosthesis has splinted all the components, the results will be different; this is perhaps the reason why external hexagon implants are still commercially available.
In the size of the implant-abutment interface, we found differences in the size of all the samples analyzed, in addition to this, we could observe that, some of the pillars, presented both vertical and horizontal mismatch as well as the study of Kano 200717; New studies should establish this fact, which is important when measuring the interfaces.
Conclusions
Dynamic loads significantly increased the discrepancy in the implant-abutment connection of both external and internal hexagon implants (p = <0.05) under the conditions analyzed; Additionally, the gap distance was greater for external hexagon implants than with Internal Hexagon implants before and after dynamic loading, being a very significant difference (p = <0.0003).
Interest conflict
The authors declare that they have no conflict of interest in the presentation and publication of this article.
Bibliografía
- Jansen V, Conrads G, Richter E. Microbial leakage and marginal fit of the implant-abutment interface. Int . J Oral Maxillofac Implants. 1997; 12: p. 527-540.
- Byrne D, Houston F, Cleary R, Claffey N. The fit of cast and premachined implant abutments.. J Prosthet Dent. 1998; 80: p. 184-192.
- Al-Turki L, Chai J, Lautenschlager E, Hutten M. Changes in prosthetic screw stability because of misfit of implant-supported prostheses. Int. J Prosthodont. 2002; 25: p. 38-42.
- Pérez Jiménez C. Evaluacion in vitro de la precisión de ajuste de pilares sobre implantes con conexión hexagonal interna y externa. In Trabajo de investigación Máster en Ciencias Odontológicas. MADRID: Facultad de Odontología Universidad Complutense de Madrid ; 2013.
- Cibirka RM NSLBRF. Examination of the implant-abutment interface after fadigue testing. J Prosthet Dent. (2001) ; 85(3):268–275.
- Costa Alves D, Perri de Carvalho P, Elias C, Vedovatto E, Ferreira Martinez E. In vitro analysis of the microbiological sealing of tapered implants after mechanical cycling. Clin Oral Invest. 2016.
- Santos A. Biomechanical study of prosthetic interfaces: A literature review.. Dental Press Implantol. 2013 Oct-Dec;7(4):90-7.
- Gil F, Aparicio C, Manero J, Padros A. Influence of the height of the external hexagon and surface treatment on fatigue life of commercially pure titanium dental implants.. Int J Oral Maxillofac Implants. 2009 Jul-Aug;24(4):583-90.
- Dias E, Bisognin E, Harari N, Machado S, da Silva C, Soares G, et al. Evaluation of implant-abutment microgap and bacterial leakage in five external-hex implant systems: an in vitro. Int J Oral Maxillofac Implants. 2012 Mar-Apr; 27 (2): 346-51.
- Tsuge T, Hagiwara Y. Influence of lateral-oblique cyclic loading on abutment screw loosening of internal and external hexagon implants. Dent Mater J. 2009; 28: p. 373-381.
- Steinebrunner L, Wolfart S, Ludwig K, Kern M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Implant Res. 2008; 19: p. 1276-1284.

Reconocimiento-NoComercial-CompartirIgual
CC BY-NC-SA
Esta licencia permite a otros entremezclar, ajustar y construir a partir de su obra con fines no comerciales, siempre y cuando le reconozcan la autorÍa y sus nuevas creaciones estÉn bajo una licencia con los mismos tÉrminos.