RESUMEN
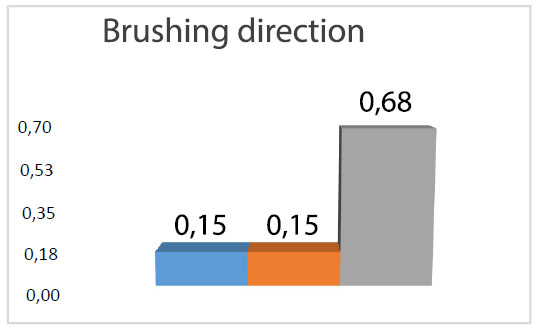
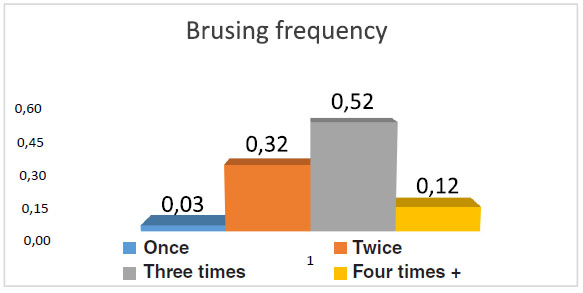
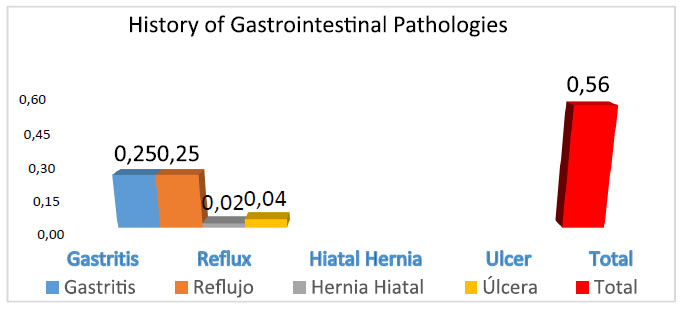
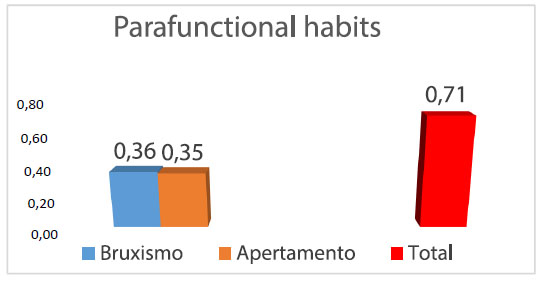
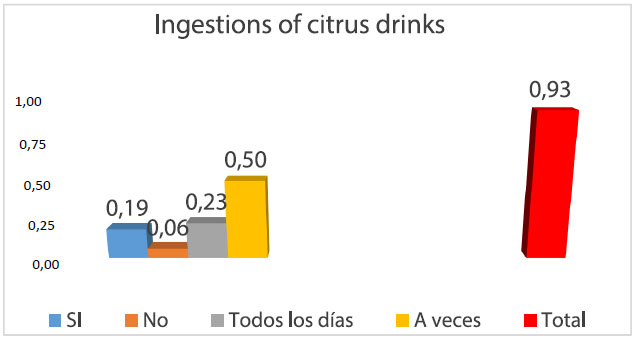
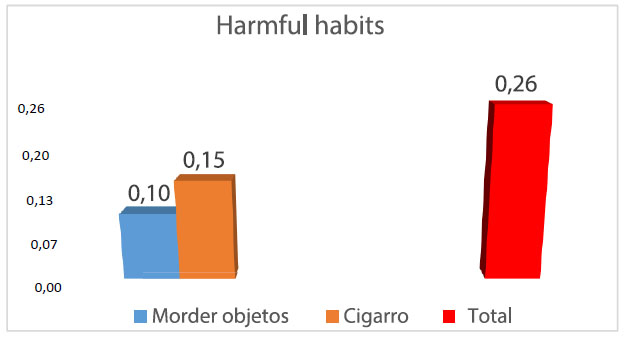
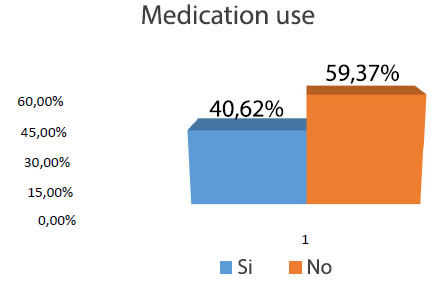
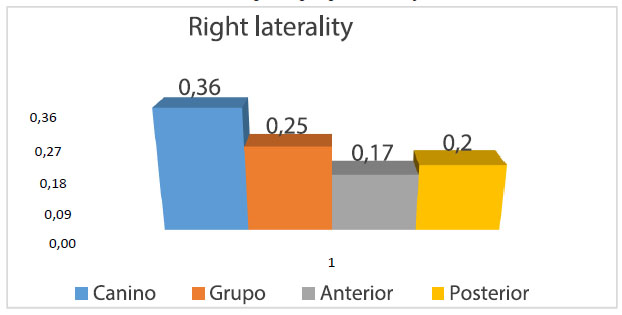
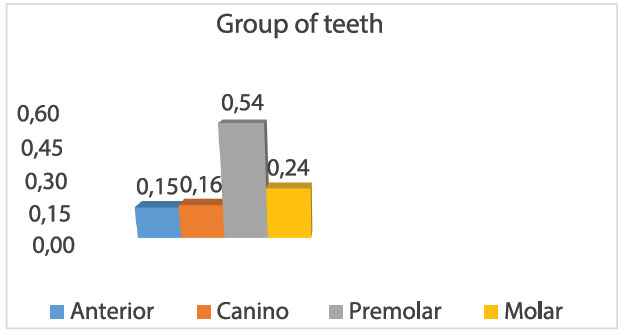
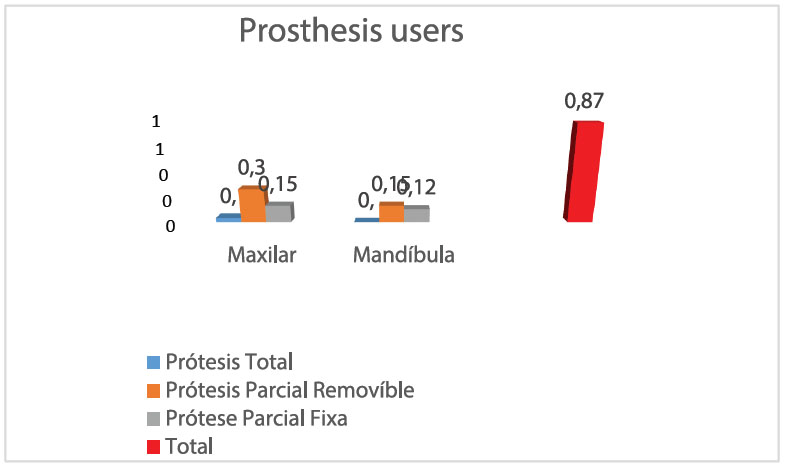
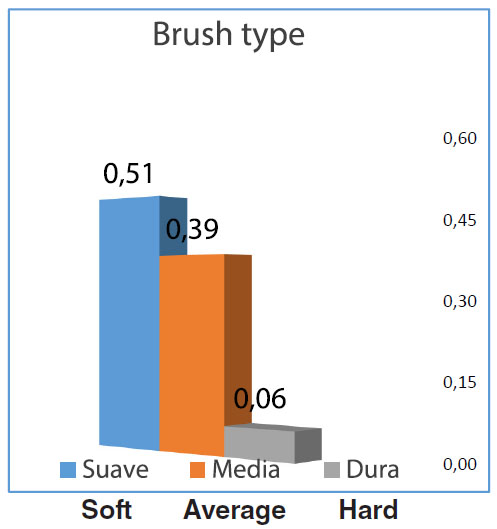
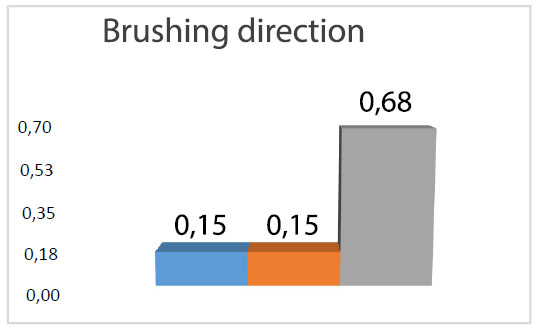
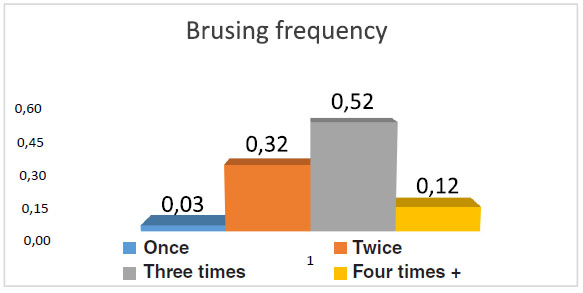
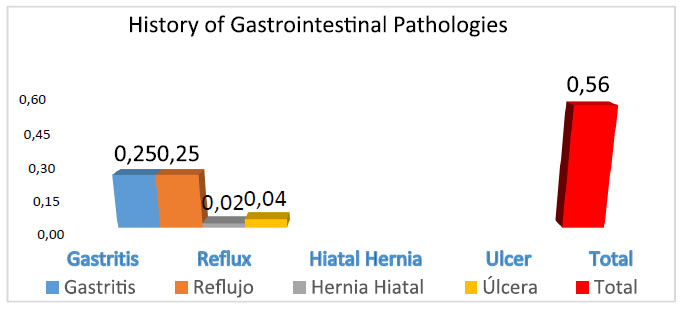
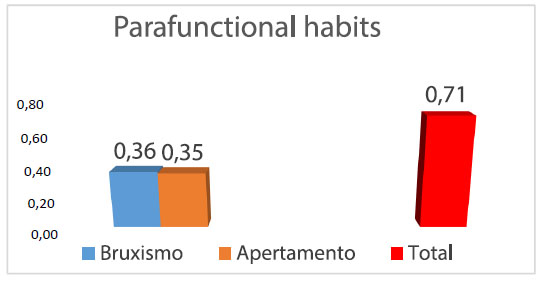
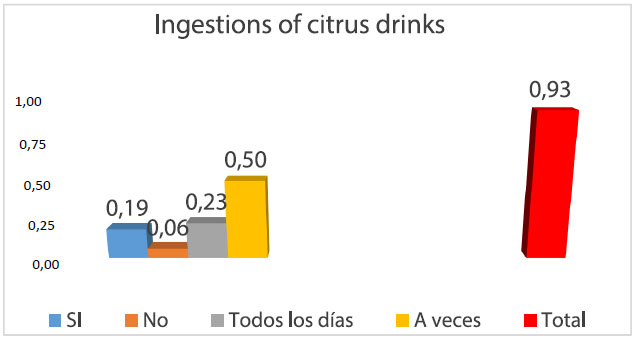
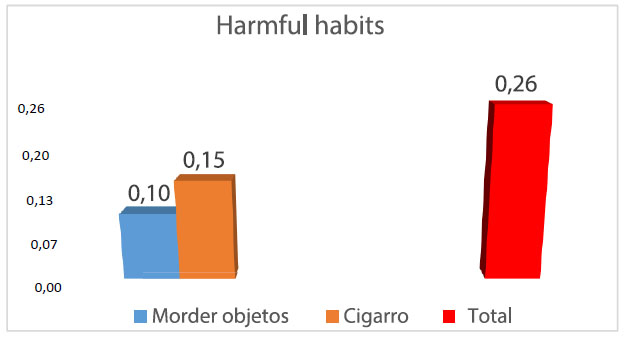
Las lesiones cervicales no cariosas consisten en la pérdida de estructura dentaria en la región cervical de la superficie vestibular de los elementos dentarios, no relacionados con caries. Objetivo: Verificar las características clínicas, epidemiológicas y los factores de riesgo de lesiones cervicales no cariosas. Materiales y métodos: Fueron evaluados 300 elementos dentarios en 96 individuos adultos que fueron sometidos a entrevista y examen clínico intra-oral. Resultados: Se encontró una razón de prevalencia en la que 0,87 de los pacientes usan prótesis. Respecto a hábitos de higiene oral, 0,51 utilizan cepillo suave; 0,52 se cepillan tres veces por día y, 0,68 utilizan dirección de cepillado combinado. En los pacientes, se evaluó que 0,56 tenían antecedentes de trastornos gastrointestinales; el 40% toman medicamentos; 0,36 presentan desoclusión en guía canina. Con relación a las características de la lesión, 0,40 presentan tipo de contacto A; 43% con profundidad inferior a 1 mm; 0,13 son portadores de prótesis parcial removible. En cuanto a hábitos alimenticios 0,93 toman bebidas cítricas; 0,15 son fumadores. Referente a los hábitos parafuncionales, 0,35 aprietan los dientes; 0,36 son bruxistas; 0,10 muerden objetos. Estas lesiones presentan una mayor prevalencia en premolares 0,54. Conclusiones: Verificando las características clínicas y epidemiológicas, y los factores de riesgo de las lesiones cervicales no cariosas, se concluye que predominan en premolares, el factor determinante para el surgimiento de estas lesiones es multifactorial, predominando la inestabilidad oclusal, ingestión de bebidas cítricas, uso de prótesis, trastornos gastrointestinales y hábitos parafuncionales.
Palabras clave: Etiología; Erosión Dentaria; Factores de Riesgo; Abrasión; Odontopatías; Bruxismo.
ABSTRACT
Non-carious cervical lesions result from the loss of tooth structure in the cervical region of the vestibular surface of the dental elements, not related to caries. With the objective to verify the clinical and epidemiological features and risk factors of these injuries were evaluated 300 dental elements on 96 adult patients that were subjected to interview and intraoral clinical examination. The results presented a prevalence ratio in which the 0,87 of patients evaluated are prosthetic users. In oral hygiene habits, 0,51 use soft brush, 0,52 brush three times a day and 0,68 use brushing direction combined. Was evaluated in these patients that 0,56 have a history of gastrointestinal pathologies; 40% made use of medications and 0,36 have disocclusion characteristics in canine guide. In relation to the characteristics of the lesion, 0,40 have type of contact, 43% with a depth less than 1 mm and 0,13 are retainers of removable partial denture. As for the eating habits, 0,93 consume citrus fruits and 0,15 are smokers. Regarding parafunctional habits, 0,35 clench your teeth; 0,36 have bruxism and 0,10 bite objects. These lesions showed a higher prevalence in premolars 0,54.Verified the clinical and epidemiological features and risk factors of non-carious cervical lesions, we conclude that the determining factor for the emergence of these lesions has shown characteristics multifactorial, with highest percentage for patients with occlusal instability, intake of acidic drinks, prosthesis, gastrointestinal diseases and parafunctional habits.
Keywords: Etiology; Toth Erosion; Risk Factors; Abrasion; Toth diseases; Bruxism.
RESUMO
As lesões cervicais não cariosas residem da perda de estrutura dentária na região cervical da superfície vestibular dos elementos dentários, não relacionados com a lesão de cárie. Objetivo: verificar as características clinicas e epidemiológicas, e os fatores de risco destas lesões. Materiais e métodos: foram avaliados 300 elementos dentários em 96 indivíduos adultos que foram submetidos a entrevista e exame clinico intra-oral. Resultados: se encontrou uma razão de prevalência em que 0,87 dos pacientes avaliados são usuários de prótese. Em hábitos de higiene oral, 0,51 utilizam escova macia, 0,52 escovam três vezes ao dia e 0,68 utilizam direção de escovação combinada. Avaliou-se nos pacientes que, 0,56 apresentam histórico de patologias gastrointestinais; 40% faziam uso de medicamentos e 0,36 apresentam características de desoclusão em guia canino. Com relação as características da lesão, 0,40 apresentam tipo de contato A, 43% com profundidade menor que 1mm e 0,13 são retentores de prótese parcial removível. Quanto aos hábitos alimentares, 0,93 consomem bebidas cítricas e 0,15 são fumantes. Referente aos hábitos parafuncionais, 0,35 apertam os dentes; 0,36 possuem bruxismo e 0,10 mordem objetos. Estas lesões apresentaram uma maior prevalência em pré-molares 0,54. Verificado as características clinicas e epidemiológicas, e os fatores de risco das lesões cervicais não cariosas, conclui-se que o fator determinante para o surgimento destas lesões demonstrou características multifatoriais, com maior percentual para pacientes com instabilidade oclusal dental, ingestão de bebidas ácidas, usuários de prótese, patologias gastrointestinais e hábitos parafuncionais.
Palavras-chave: Etiologia; Erosão Dentária; Fatores de Risco; Abrasão; Odontopatias; Bruxismo.
INTRODUCTION
Non-carious cervical injuries (LCNC) are injuries that result from the loss of dental structure in the cervical region not related to caries injury. It has a multifactorial etiology; the combinations of factors contribute to the cause of the problem, so it is considered complete for both the studio and the treatment¹. The etiological factors of this injury may be abrasion, erosion, friction, friction or asociation2-5.
The LCNC reside in a group of more complex lesions in the dental clinic, mainly in the identification of the causative agent and the treatment offered. Several factors may contribute to the appearance and development of these lesions, but they do not necessarily act as a direct cause of them. Knowledge of the etiology of these lesions is essential for effective and safe treatment, as well as to help prevent the development and progression of new lesions6.
Clinical studies are critical to clarify and validate hypotheses of how LCNCs are initiated, providing a solid basis for clinical diagnoses7. The perception and impact of the mechanisms of injury and their interactions become an effective guide for clinicians to evaluate their patients8,9.
The mechanical maintenance of oral hygiene can contribute taking into account that the direction and intensity of the forces applied to the teeth are important factors for the appearance10,11, age and sex can influence the prevalence of injuries12.
Occlusion is another important factor. The stress on the interface of the enamel and dentin at the junction of the cement enamel may allow the appearance of LCNC13,14. Diet is another factor in the appearance of lesions15.
The objective of this study was to verify the clinical and epidemiological characteristics, as well as the risk factors of LCNC in adult individuals.
Material and method
The study was presented to the Research Ethics Committee of the Metropolitan University of Santos, UNIMES and approved under the number 1,809,698. Ninety-six individuals were evaluated and interviewed for epidemiological analysis and intraoral clinical examinations to evaluate the clinical characteristics of 300 teeth with non-carious cervical lesions. People with one or more dental elements with non-carious cervical lesions were included in the study. Individuals with bimaxillary total prosthesis and under 18 years were excluded from the study.
The interviews and the clinical examination were applied by a previously trained examiner to avoid possible reading errors.
The interviews were designed to analyze the following aspects: gender, use of prostheses, brush type, brushing direction, history of gastrointestinal disorders, frequency of eating or eating acidic foods, history of harmful habits, history of parafunction and daily medication use. For the intraoral clinical examination, clinical clamps (Duflex®), scanner (Duflex®), mirror No. 5 (Duflex®), Palmer clamp (Duflex®), millimeter scan probe No. 1 (Duflex®), articulation paper were used in strips (Accufilm ll).
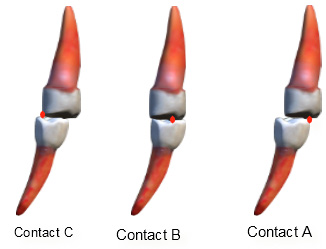
For the analysis of the types of occlusal contact points in the oral-lingual LCNC support elements, contacts of three types were analyzed: Contact A (crushing slope of the upper teeth in contact with the smooth slope of the lower teeth); contact B (crushing slope of the upper teeth against crushing slope of the lower teeth and contact C (smooth slope of the upper teeth with crushing slope of the lower teeth). Certain records of contact points were analyzed in all LCNC elements by means of of carbon strips and Palmer clamps (Duflex®) with patients positioned maxillary-mandibular relationship of central occlusion (Figure 1).
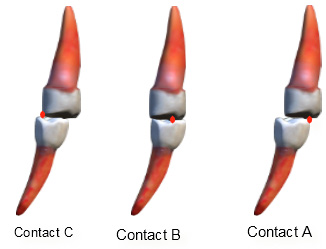
Figure 1. Illustration of contact points
For the analysis of the occlusive guides, the visual evaluation was used and confirmed by paper to articulate in strips (Figure 2)

Figure 2. Deocclusive guide - Right Laterality
The characteristics of the injury were analyzed by means of a millimeter probe placed in the center of the injuries and perpendicular to the long axis of the tooth, according to the Index of dental wear proposed by Smith and Knight (Figure 3)16.

Figure 3. Depth of the Injury
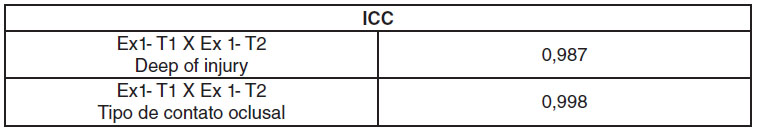
The intra-examiner error was calculated with CI (> 95%) by the Kappa method to observe the intra-examiner agreement by repeating the measurements and recording the contacts. All tests were tabulated and their results expressed in tables.
Results
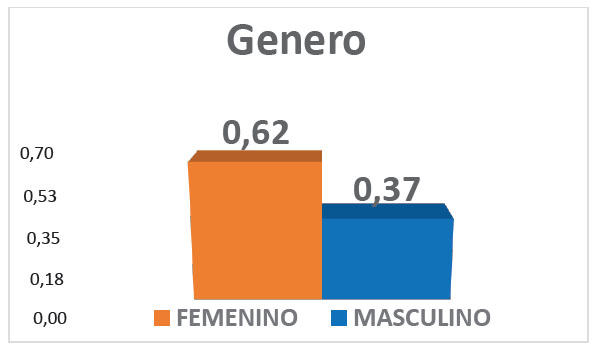
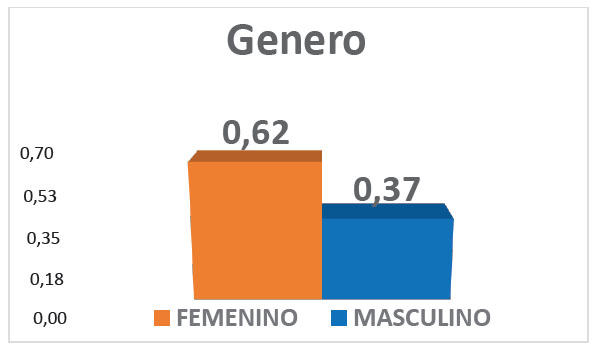
Regarding to the female and male gender, there was a significant prevalence for the female gender (Figure 1) with a prevalence ratio (PR) of 0.62.
Picture 1. Prevalence ratio regarding gender
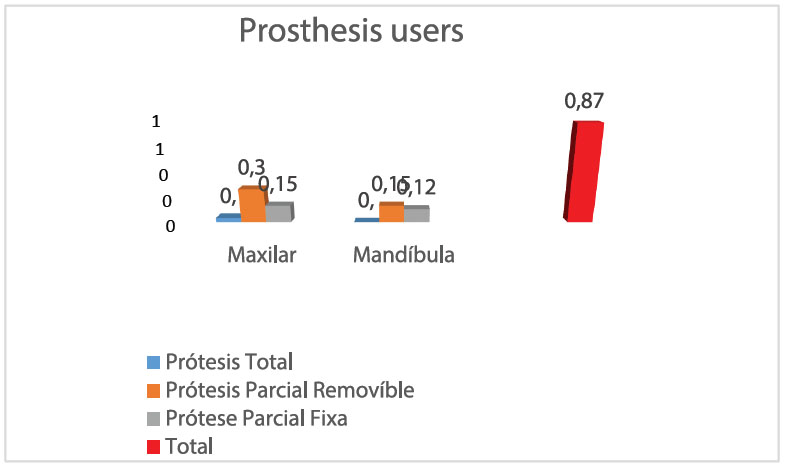
There was a significant prevalence among prosthetic users (Graph 2) and the presence of LCNC with a PR of 0.87. Among the evaluated patients who used some type of prosthesis, the prevalence of partial removable prosthesis users with RP of 0.45.
Picture 2. Prevalence ratio for prosthetic users
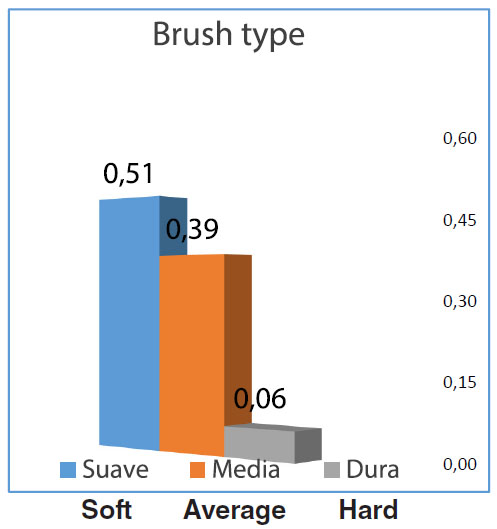
Regarding to oral hygiene habits, the following questions were asked: the type of hair used was soft, medium or hard bristles (Graph 3); the frequency of daily picks varied once a day, from time to time, three times and four times the worst (Graph 4); type of zip direction performed with horizontal, vertical and combined movement (Graph 5).
No significant changes were found in the results regarding the presence of the lesion and oral hygiene habits
Picture 3. Prevalence ratio regarding the type of brush
Pcture 4. Reason for prevalence regarding brushing direction
Picture 5. Prevalence ratio regarding Brushing Frequency
Regarding to the history of gastrointestinal disorders (Graph 6), there was a significant prevalence in patients with gastrointestinal disorders and the presence of LCNC with RP of 0.56.
Picture 6. Reason for prevalence regarding the History of Pathologies
Regarding to parafunctional habits (Graph 7), a high prevalence was observed that associates these habits and the presence of LCNC with RP of 0.71. Among those evaluated, bruxism prevailed with a PR of 0.36.
Picture 7. Reason for prevalence in reference to Parafunctional Habits
Regarding to eating habits, this study investigated the relationship between the intake of acidic drinks, fruits and / or citrus juices with the presence of LCNC (Graph 8). There was a high prevalence of acid consumption habits and the presence of LCNC with PR of 0.93.
Picture 8. Reason for prevalence regarding ingestion of acidic beverages
Regarding to harmful habits (Table 9), there was no high prevalence of these habits and the presence of LCNC, with RP of 0.26.
Picture 9. Reason for prevalence regarding harmful habits
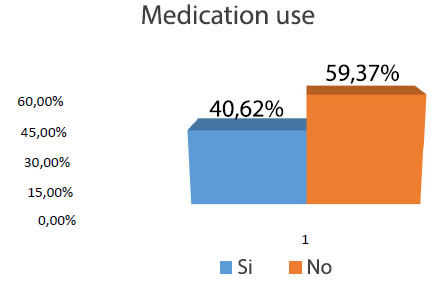
Regarding to the use of medications, the present study did not find a significant prevalence between the use of medications and the presence of LCNC (Graph 10), with a PR of 0.40.
Picture 10. Percentage in relation to the use of medications in Systemic conditions
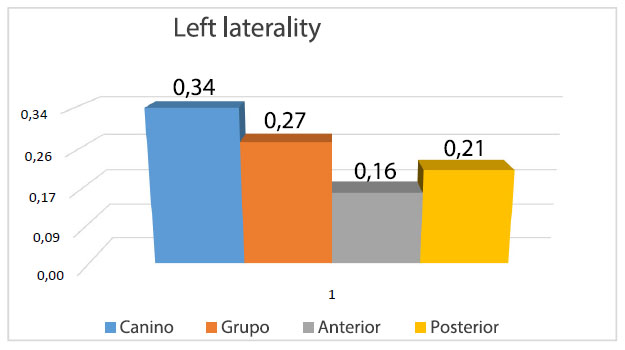
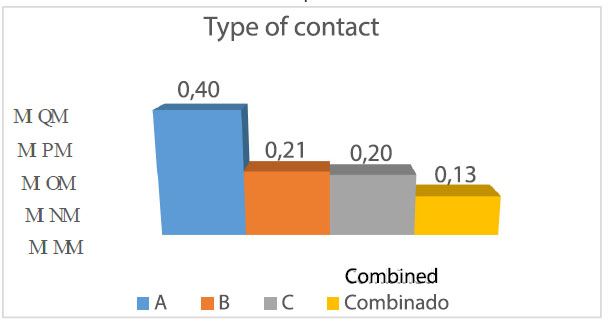
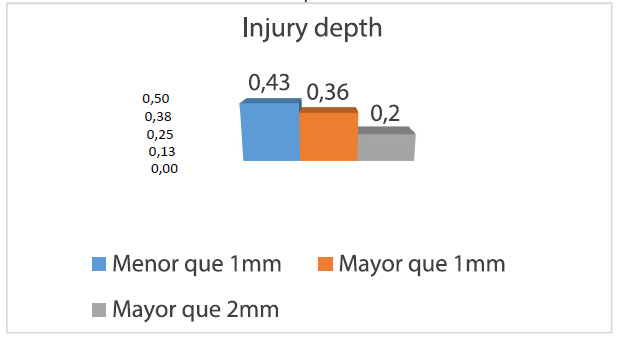
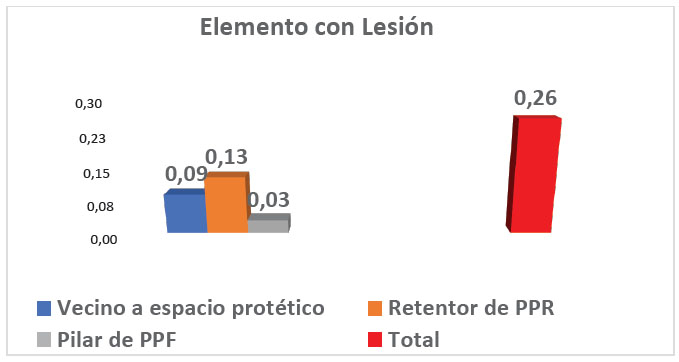
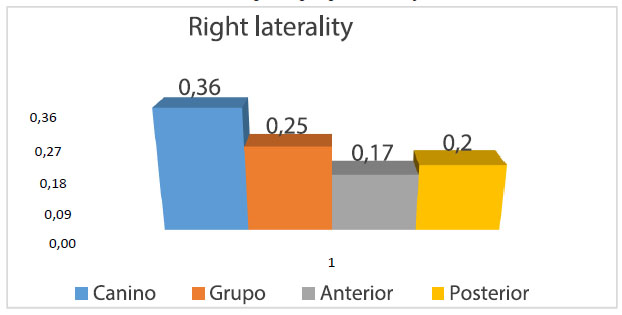
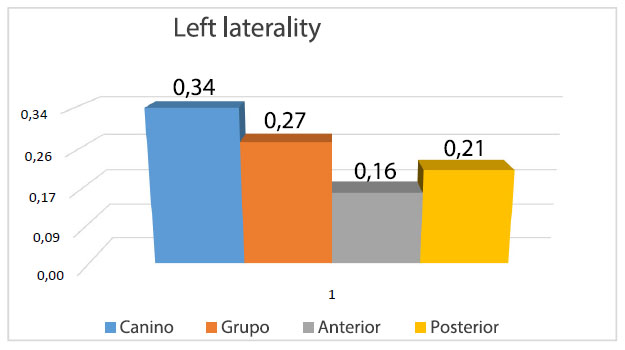
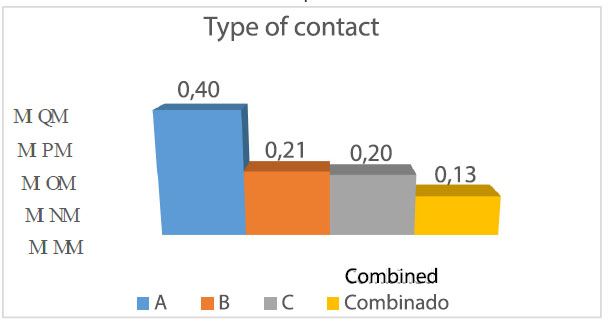
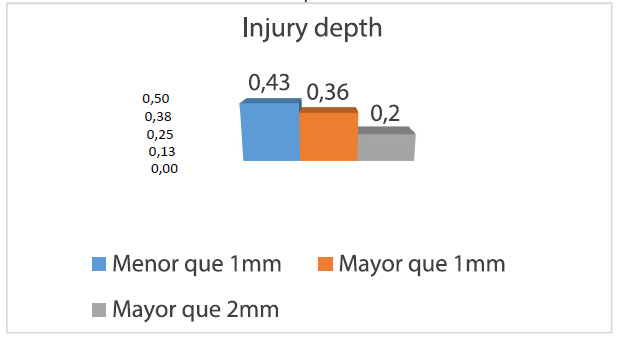
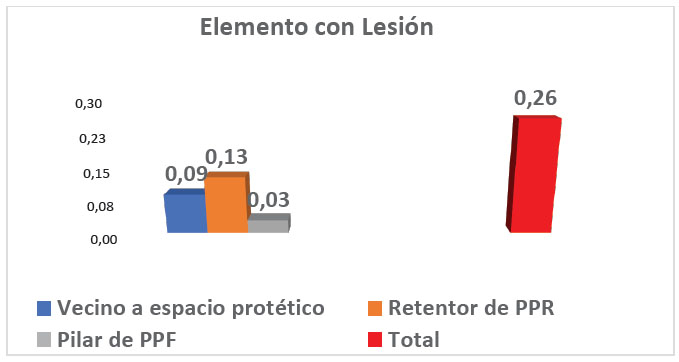
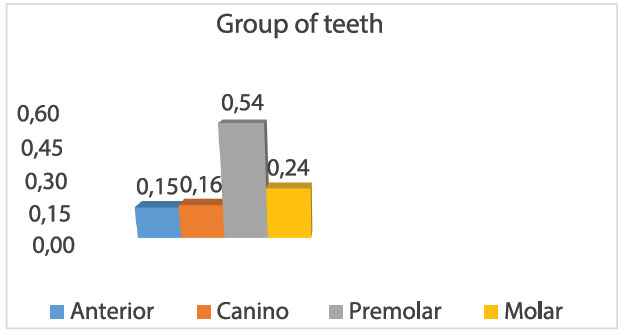
Intraoral examinations containing the following "characteristics" were performed: deocclusion movements, right laterality (Graph 11) and Left (Graph 12); the types of occlusal contacts A, B, C and combined (Figure 13); The depth of the lesion is less than 1 mm, greater than 1 mm and greater than 2 mm (Figure 14); with respect to the elements with cervical lesion as a removable partial denture retainer (PPR), adjacent to the prosthetic space and fixed partial prosthetic abutment (PPF) (Figure 15), and with respect to the group of teeth that are anterior, canine, premolar and molars (Graph 16).
There was an expressive prevalence with respect to occlusion characteristics in the lateral movements of the canine guide and the presence of LCNC (Graphs 11 and 12) with a PR of 0.98.
Picture 11. Prevalence ratio regarding Right Laterality movements
Picture 12. Prevalence ratio regarding the movements of the left laterality
Regarding the types of contact, there was a significant prevalence of occlusal instability and the presence of LCNC (Figure 13), with a PR of 0.94. Among the elements evaluated with occlusal instability, there was a greater predominance for A contact with RP of 0.40.
Picture 13. Razón de prevalencia referente a los tipos de contatos
In the characteristics of the lesion regarding to depth, a higher prevalence was observed for the defect less than 1 mm deep (Graph 14), with a PR of 0.43.
Picture 14. Percentage in relation to injury depth
Picture 15. Prevalence ratio referring to the elements with LCNC.
The evaluation of the group of teeth (Graph 16) showed a high prevalence of premolars and the presence of LCNC with PR of 0.54.
Picture 16. Razón de prevalencia referente al grupo de dientes; Prevalence ratio regarding the group of teeth
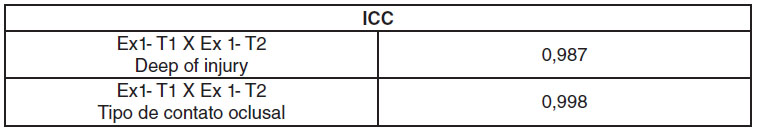
Reliability fo the measurement
With respect to the measurements of the depth of the lesion and the types of occlusal contacts, performed in 2 moments (T1 - first moment as a complete sample; T2 - 30 days after the first registration) for 20 patients to assess the reliability of the data Registered patients were analyzed by intraclass correlation (ICC).
Table 1: Reliability of assessments for depth of injury and types of occlusal count using ICC
Discussion
Analyzing the results obtained in 96 patients with cervical lesions, it is found that, with respect to gender, there was a significant prevalence of women, with a prevalence rate of 0.25 more than men. Some studies have reported a higher prevalence in men10,12 and in other gender studies was irrelevant15,19.
With regard to the type of prosthesis, in the hub related to the type of retention of the PPR with the LCNC20. In this study, the users of prostheses had a significant prevalence of 0.87, being more prevalent in PPR with 0.46.
As for oral hygiene habits, in the hub a direct relationship with the presence of cervical injuries, as well as the frequency and direction of the spine, which depends on the association with other factors related to the presence of cervical injuries, such as corroboran some authors4. In another study it is found that the manual belt has a higher prevalence in the gingival recession with the use of hard pins5 as compared to an electric belt11.
Regarding to gastrointestinal upheavals, this studio will find that there is a relationship between gastrointestinal upheavals and the presence of LCNC. Another studio coincides with the result of this work18 indicating that patients with gastric reflux are more susceptible to mechanical wear.
With reference to parafunctional habits, studies indicate a direct association with these habits and the presence of LCNC3,5. The collaboration with these studies identified that there is a relationship between parafunctional habits and injuries, presenting the result of a prevalence table 0.36 for bruxism and 0.35 for presentation.
As far as food habits are concerned, researchers investigated the link between cold carbonated drinks, fruits and fruit juices with the LCNC formation, but there was no correlation between them4. In contrast, in this study there was a significant prevalence among the consumption of acidic foods and the presence of non-carious cervical injuries, where 0.93 of the analyzed patients contain this habit.
With regard to harmful habits, in this studio in the hub a direct relationship with the LCNC, however, in another studio hubo a relationship between the LCNC and the harmful habits, in which 58% of the subjects bite objects and 21 % were cigarettes consumers5.
Regarding the use of medications, I cannot relate to the presence of LCNC with a prevalence ratio of 0.40, however, another study describes that the intake of medications increases hyposalivation and interferes with the pH of the saliva, causing more acid and increase in dental wear17.
As for the characteristics of the occlusion, a study found that 63% of patients evaluated with LCNC had group function guidance in lateral mandibular movements, concluding that the direction and intensity of strength applied to patients could be contributing to them. the appearance of the students. cervical lesions not carious10. In this study, with respect to the orientation of the group function in the mandibular movements of the lateral side, there was a prevalence rate of 0.70 of the lesions occurred in the canine guide, no, however I have a direct relationship with the cause of the injury.
In the elements with cervical injury, the investigation showed a high prevalence with respect to the instability of dental occlusion, with a predominance in contact A containing 0.40, followed by contact B of 0.21 and contact C with 0.20. However, horizontal strengths were exactly harmful because they generate contact and discharge strengths. Another study collaborates with the results obtained in this study that the lateral and occlusal strengths cause the flexion of the cusp and the causes of the rupture of the dental structure in the cervical region21.
With respect to the injury depth factor, in the present study, a higher prevalence in defects of depth of less than 1 mm was identified in elements with LCNC, another studio also found an increase in the prevalence of injuries in depth of less than 1 mm3, The elements with a minimum contour loss and defects of less than 1 mm must remain under regular dentist control. Injuries with larger defects of 1 mm and 2 mm in depth need restorative treatment18.
Finally, with respect to the group of patients, the present study shows that 0.54 of the patients evaluated have the highest concentration of LNC in premolars and molars. Other studies coincide that the largest group of affected teeth were premolar and molar3,4,10,15.
Conclusion
According to the results obtained in this study, it is possible to conclude that people with a lesion depth less than 1 mm, alcohol consumption habits, users of dental prostheses, people with parafunctional habits and people with gastrointestinal upheavals a high prevalence of LCNC. Therefore, indicate that the etiology of these injuries is multifactorial.
Bibliografía
- Baratieri LN, et al. Odontologia Restauradora: Fundamentos e Técnicas. Gen Grupo Editorial Nacional. Ed Santos SP 2010; p 760.
- Perez CR, Gonzalez MR, Prado NAS, Miranda MSF, Macedo MA, Fernandes BMP. Restoration of noncarious cervical lesions: when, why, and how. Inter J Prosth Dent 2012; 8 (10); 2-8.
- Boric J, Anic I, Urek MM, Ferreri ES, The prevalence of non-carious cervical lesions in permanent dentition. J oral rehabil 2004; 117 – 123.
- Oliveira ACS, Damascena NP, Souza CS. Análise clínica de pacientes portadores de lesões cervicais não cariosas e sua relação com hábitos. Rev Sul-Bras Odontol 2010 Jun; 7(2):182-92.
- Lima LM, Humerez Filho H, Lopes MGK. Contribuição ao estudo de prevalência, do diagnóstico diferencial e de fatores etiológicos das lesões cervicais não-cariosas. RSBO. Sul-Bras Odont 2005; 2 (2); 17-21.
- Barbosa RPS, Santos RL, Gusmão ES. Terapias para controle de lesões não cariosas hipersensíveis. Odont Clín Científ set/dez 2005; 4 (3): 171-176.
- Nguyen C, Ranjitkar S, Kaidonis JA, Townsend GC. A qualitative assessment of non--carious cervical lesions in extracted human teeth. Aust Dent J 2008 Mar;53(1):46-51.
- Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspective on tooth surface lesions. J Am Dent Assoc 2004 Aug;135(8):1109-18; quiz 1163-5.
- Litonjua LA, , Andreana S, Bush PJ, Cohen RE. Tooth wear: attrition, erosion and abrasion. Quintessence Int 2003; 34; 435-446.
- Brandini DA, Lunardeli CT, Panzarini SR, Pedrini D. Clinical evaluation of the association between noncarious cervical lesions and occlusal forces. Rev J Prosth Dent 2012 November; 108: 299-303.
- Heasman PA, Holliday R, Bryant A, Preshaw PM. Evidence for the occurrence of gingival recession and non-carious cervical lesions as a consequence of traumatic toothbrushing. J Clin Periodontol 2015; 42 (16): 237–255.
- Lordanishvilia AK, Chernyjb DA, Yankovskijb VV, Orlovc AK, Drobkovac KO. prevalence of noncarious hard dental tissue lesions in adults at various age periods. Adv in Geront 2015; 5 (4): 298–302.
- Poiate IA, Vasconcellos AB, Poiate E Jr, Dias KHC, Stress distribution in the cervical region of an upper central incisor in a 3D finite. Braz Oral Res 2009; 23(2): 161-7.
- Romeed SA, Malik R, Dunne SM. Stress analysis of occlusal forces in canine teeth and their role in the development of non-carious cervical lesions: abfraction. Inter J Prosth Dent 2012; Artic ID 234845, p 7.
- Sawlani K, Lawson NC, Burgess JO, Lemons JE, Kinderknecht KE, Givan DA. Factors influencing the progression of noncarious cervical lesions: A 5-year prospective clinical evaluation. Rev J Prosth Dent 2015; 1-7.
- Smith BG, Knight JK. Na index for measuring the wear of teeth. Br Dent J. 1984 jun 23; 156(12):435-8.
- Michael JA, Townsend GC, Greenwood LF, Kaidonis JÁ. Abfraction: separating fact from fiction. J Aust Dent 2009; 54: 2–8.
- Jakupovic S, Cerjakovic E, Topcic A, Ajanovic M, Konjhodzic PA, Vukovic A. Analysis of the abfraction lesions formation mechanism by the finite element method. ACTA Inform Med 2014 Aug; 22(4): 241-245
- Telles D, Pegoraro LF, Pereira JC. Prevalence of noncarious cervical lesions and their relation to occlusal aspects: a clinical study. J Esthet Dent 2000; 12(1):10-5.
- Luthi LF, Santos MBF, Henriques GEP, Barbosa CMR. Odontogeriatria e as Lesões não Cariosas. UNOPAR Cient Ciênc Biol Saúde 2010;12(4):37-40.
- Vasudeva G, Bogra P. The effect of occlusal restoration and loading on the development of abfraction lesions: A finite element study. J ConservDent. 2008 Jul;11(3):117-20

Reconocimiento-NoComercial-CompartirIgual
CC BY-NC-SA
Esta licencia permite a otros entremezclar, ajustar y construir a partir de su obra con fines no comerciales, siempre y cuando le reconozcan la autorÍa y sus nuevas creaciones estÉn bajo una licencia con los mismos tÉrminos.