INTRODUCTION
Fifth-class cavitary lesions are found in the gingival or cervical third of the buccal or labial and lingual faces of all teeth in patients with occlusal problems, bruxism, poor hygiene, consumption of citrus foods, smoking and in the elderly advanced These lesions can affect dental sensitivity, plaque retention, incidence of caries, structural integrity and vitality of the pulp, and cause greater gingival irritation if we find them in the anterior region; In addition, they can cause aesthetic and functional problems. They are often associated with gingival recession, causing structural weaknesses reflected in a poor relationship between crown and root1. Despite its high prevalence in the world population, dentistry has not been able to establish standards for its diagnosis and adequate treatment of these alterations or problems, thus representing a challenge for its successful restoration2,3.
For a long time, a suitable biomaterial has been sought, which within its properties resembles dentin and possesses the mechanical, aesthetic, biocompatibility characteristics to ensure gingival reinsertion, and adequate properties for retention4. That is, it has excellent adhesion to the tooth, thus achieving resistance to oral microfiltration of liquids, caries inhibition and ease of handling, since microfiltration can have consequences such as: dental hypersensitivity, pulp irritation, bacterial plaque deposit; In addition, bacteria pass through the margin of restoration that can cause recurrent caries and contribute to the corrosion, dissolution or discoloration of these materials1,3,4.
There are many discrepancies regarding fifth-class restorations because it is a place of difficult access and little mechanical retention for the restoration biomaterial5,6. There is a high failure rate due to the difficulty of isolating the area undergoing gingival tissue restoration and poor adhesion of biomaterials to dentin and root surfaces1.
The glass ionomer has several advantages such as high adhesion to the dental structure thus sealing the cavity, which provides protection to the pulp, ability to adhere to the dental structure, elimination of secondary caries and the prevention of microfiltration in the margins. Apart from releasing fluoride without affecting the physical properties of cement3.7.
Composite resins have been widely used as restorative material in dentistry because of the aesthetic demands of the patient. Constantly, new formulations are introduced with the aim of improving their mechanical and physical properties such as decrease in particle size, increase in radiopacity, changes in the shape and distribution of their charge particles. However, they have limitations such as: microfiltration associated with polymerization contraction, which are the most cited reasons for failure in restorations with said material8.
The advantages of the composite resin are the potential to overcome the marginal gaps that occur due to contractions of the materials, as well as greater resistance to fracture and wear, as well as greater biocompatibility9.
The use of glass ionomer or Nano particulate composite resin in fifth class restorations is a controversial issue, since the greatest failures are reported in this type of restorations, since the use of dental biomaterial should be adequate since it should allow good marginal adaptation avoiding deterioration6. This study aims to identify the degree of in vitro microfiltration of the glass ionomer and the composite resin in non-carious class V lesions.
Materials and methods
This study was conducted at the Pros mile Clinic, Metropolitan Hospital and University of the Americas as a randomized experimental approved by the Ethics and Bioethics Committee of the University of the Americas No. 2014-0803, Quito-Ecuador. The sample was made up of 80 healthy premolars extracted for orthodontic reasons, obtained by donation by dentists, after the signing of the informed consent. For the study, all teeth with dental caries, with the presence of fillings or with some type of dental anomaly were excluded. The extracted teeth were cleaned and preserved in 0.9% sodium chloride at 37° C for 60 days prior to the study10. Before the preparation of the cavities, the dental surfaces were cleaned with a mixture of pumice powder prepared with distilled water, using a prophylactic brush (Prehma®, NJ, USA) and contra-angle (NSK®, Japan) of 8,000 rpm for 2 seconds. On the vestibular surface of each dental piece, a fifth-class freehand wedge-shaped cavity resembling an injury (abrasion, erosion and abfraction) was made, for this a cylindrical bur of coarse-grained diamond No. 0 was used, 12 (coolcut, MDT, Israel) at high speed with an NSK® turbine (Japan). Each bur was changed after having made 5 preparations. Class V cavities had the following characteristics: 1.5 mm deep x 3 mm high in the occlusion-gingival direction x 2 mm in the mesio-distal direction, which extended to approximately 1 mm below the amelocementary limit. A graduated periodontal probe from William (GDC, India) was used to confirm the dimensions of the cavity11. All preparations were randomly divided into two groups (n = 40): 1) glass ionomer and 2) nanoparticulate composite resin.
Cavity restoration
Prior to this process, the cavities were cleaned with a prophylactic brush, pumice stone, distilled water and contra-angle at 8,000 rpm for 20 seconds. Subsequently, it was washed with abundant distilled water and dried with a triple syringe for 15 seconds, removing excess distilled water.
Group 1, Ketac Molar® Easy mix (3M ESPE)
According to the manufacturer's instructions, the bottle was shaken to allow the powder to flow freely, a mixing portion (unit of weight) of 4.5 parts of powder, a level meter and level of liquid (1 drop) was used. Sufficient amounts of powder and liquid were dosed in the mixing block by keeping the liquid in an upright position during dosing to avoid air bubbles. Polyacrylic acid (Universal Etchant: Ref 665951 Lot: 44000188332/01, 3M Germany) was applied at 10% for 20 seconds12, followed by washing with distilled water for 30 seconds and dried with a sterile cotton swab of 0.5 mm Subsequently, the Ketac Molar Easy mix (Ref 453765 Lot: 43567853G87, 3M, Germany) was applied in several portions using a plastic gutta-perchero (Maillefer). The entrapment of air bubbles in the enamel cut was avoided. The cavities were obtained and the indications of the supplier that indicated using petroleum jelly to properly disperse the material were followed. Then, the finger was removed sideways preventing the material from detaching. Finally, we waited for the material to set.
Group 2 Composite resin Z350 XT (3M)
According to the manufacturer's instructions, etching was carried out with orthophosphoric acid (Ref 665951 Lot: 44000188332/01, 3M Neuss-Germany) at 37% for 15 seconds in enamel and dentin. The acid was cleaned with air / water for 20-30 seconds. Subsequently, the cavity was dried with a 0.5 mm swab, the enamel obtained an opaque white color, indicative of a good engraving. Then, Adper® adhesive, single bond 2 (Ref 51202 Lot N 7302462018-10, 3M, USA) was applied with a microbrush (applicator), evaporating the solvent with air from the triple syringe. One more layer of adhesive was placed and polymerized in 20 seconds with the halogen light lamp with a wavelength wavelength 375-510 nm (Litex 680th Dentamerica, USA) (12,13). Next, approximately a 3 mm layer of Z350 XT resin (Ref 7018A2B Lot N808795, 3M, U.S.A) was placed, using an incremental technique on the piece to be restored with a metal bur until the cavity is fully restored. It was light cured for 20 seconds after each resin application. Finally, in the last placement, liquid glycerin was used to remove the hybrid layer. The restorations were finished and polished using sof-lex-pop-on discs (3M ESPE).
Sample preparation after thermocycling process
Once the restorations were made, the premolars were submerged in distilled water (German apothecary) simulating the saliva, until the materials have finished their setting process (glass ionomer) and the nanoparticulate resin obtains its correct marginal seal7,14. Twenty-four hours later, transparent nail varnish (Vogue) was placed 2 mm away from the restoration. Once dry, the teeth were immersed in 2% methylene blue for 7 days at a constant temperature of 37° C (without changing the solution). Then, the samples were placed in 1.5 ml microtubes with 0.05 ml of methylene blue (German pharmacy) and 100 ml of distilled water. These were introduced in a thermal cycler (MultiGeneTM Mini Personal Thermocycler, Labnet, NJ, USA) to simulate thermal changes of 37 °, 72° and 75° C for 8 hours and 45 min each cycle with a duration of 17 seconds and for a total of 500 cycles, in order to produce expansive and compressive forces which generated fatigue and wear of the restored material. These fluctuations in temperature simulate various events that occur in the mouth.
Observation of samples in the stereomicroscope
After the thermo cycling process, the apices were sealed with self-healing acrylic (Vivadent) and once again a thin layer of varnish was placed 2 mm from the restoration. When the varnish was dried, the samples were immersed in a solution of 2% methylene blue for seven days at a constant temperature of 37°C. Then, the pieces were washed with circulating drinking water for 3 hours to clean the excess dye. Longitudinal sectioning was carried out with diamond disk without refrigeration and micro motor (Buffalo power, United States at 45,000 rpm). Once this process was finished, samples that at the time of histological cutting have been altered the restoration, also those that do not retain the required staining and those that have suffered an alteration or fractures during manipulation were excluded.
The gingival part was observed with a stereomicroscope (Leica M60 Biosystems, USA) according to the following scale:
- Grade 0: Absence of microfiltration.
- Grade 1: Marginal Filtering.
- Grade 2: Marginal restoration filtration up to the middle third.
- Grade 3: Marginal filtration of the restoration to the bottom.
Statistics analysis
The samples were described and tabulated according to the categorical variables of degree of filtration and type of material. The results were analyzed with the chi-square statistical test in the SPSS 24® program. Values below 0.05 were taken as significant.
Results
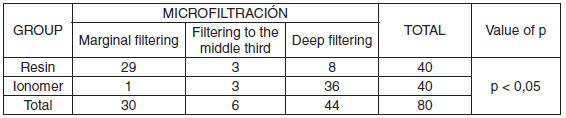
The data obtained from the observation through the microfiltration steromicroscope in the dental pieces were summarized in Table 1 and the degrees of microfiltration of Z350 XT resin (Figure 1) and those of ionomer (Figure 2).
Table 1. Microfiltration observed in Z350 XT resin and Ketac Molar easy mix glass ionomer.
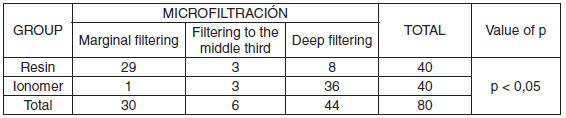
55% of the test tubes in which Z350 XT Resin was used showed marginal filtration of the restoration.
1.- 27.5% presented marginal filtration of the restoration (Grade 1).
2.- 17.5% marginal filtering of the restoration and filtration to the middle third of the restoration (Grade 2).
Trend contrary to that presented by the glass ionomer
1. 12.5% presented marginal filtering of the restoration (Grade 1).
2. 20% of the specimens presented marginal filtration up to the middle third of the restoration (Grade 2)
3. 67.5% marginal filtering, edge and bottom of the restoration (Grade 3).
Figure 3 shows the comparison between these two materials.
Comparatively, differences in the degree of microfiltration are observed for the two dental biomaterials used in the treatment of non-carious V lesions, while with the Nano particulate resin only 17.5% presented grade 3 microfiltration, with the glass ionomer the reference was 67.5%.
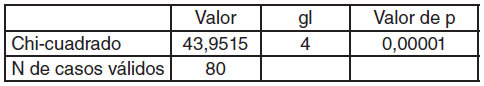
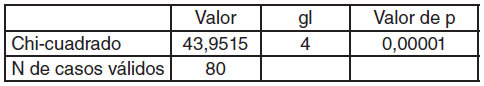
By means of the chi-square test, it was possible to determine that there was a significant difference in the degree of microfiltration related to the type of biomaterial used (p = <0.00001), with which it can be asserted that the Nano particulate resin produces less microfiltration than the ionomer of glass (Table 2).
Table 2. Results of chi square test for microfiltration grade.
Discussion
In the present study the alternative hypothesis was accepted, the results show how the resin has less filtration than the glass ionomer. The main reasons for the failure of compounds such as glass ionomer and resin are interfacial defects that develop as a result of long exposure to thermal and mechanical stresses, stress developed due to polymerization contraction and physical and chemical properties of the material. These interfacial defects can lead to microfiltration, which is a cause for concern, as it can lead to discoloration, recurrent caries, pulp inflammation, post-operative sensitivity, periodontal problems and nionomerecrosis4,15. Many attempts have been made to prevent the recurrence of microfiltration at the interfaces of the restorations to prolong longevity16.
Microfiltration is an important property that has been used in the evaluation of the success of any restorative material. Despite the great advances that have been made on microfiltration in class V restorations, they are still the great weakness in restorative dentistry. Several in vitro studies have been carried out over the past few years, which are the best way to simulate the reality of the oral cavity. Unfortunately, these studies do not reveal exactly the dental physiology, but they do help us and are a basic element for further studies. The dental biomaterials used in this project are quite effective and the most used by the vast majority of dentists. However, the material with which it works, the technique of placement and indications of manufacturers are determining factors for the success in the restorations, as well as the duration of the same16,17.
The results suggest that the techniques used show statistically significant differences in their microfiltration values. The Ketac Molar glass ionomer showed the highest filtration while the lowest values were those of the Z350 XT resin. However, in some studies different results were found than ours with respect to the Ketac Molar glass ionomer, these discrepancies can be attributed to the handling of the materials in operative times18.
The results of this investigation lead to the fact that none of the proven restoration materials were able to seal the margins or the walls of the teeth completely. This may be related to: a) improper fit between the tooth or the restoration materials and b) the mechanical properties of the fixing cement, that is, a poor adhesion between the cement materials and the core3. However, in this study it was confirmed that in class V restorations with the Nano particulate resin there is greater resistance to microfiltration than the glass ionomer since filtrations were less frequent in the enamel margins than at the edge and bottom (Figure 3).
The lower degree of microfiltration could be due to the fact that the resin has a high adhesive strength, produced by 2 important factors: a) phosphoric acid which helps eliminate the smear layer and thus increase the bond strength and improve the adaptation of the compound. The fourth generation adhesive has a Nano fill load that allows a homogeneous layer to be formed and more stable to dimensional changes. Due to the variations in temperature and the contraction resulting from polymerization, it gives the restoration different characteristics, making it more effective in preventing microfiltration and b) it has lower viscosity and low modulus of elasticity of Nano metric particles19.
Improvements in composite resins have increased their usefulness as restorative materials; however, polymerization contraction continues to be one of its main deficiencies15. The ideal material would be one that chemically joins the structure of the teeth4. This contraction causes stress within the restoration and the surrounding dental structure that leads to leaks20. Possible reasons for microfiltration in the margin of dentin restoration are the cavity configurations (factor C), the orientation of cervical wall dentin tubules (CEJ), the organic content of the dentin substrate and the movement of dentinal tubular fluids, incomplete alteration or elimination of the smear layer by acidic primers for proper demineralization and formation of the hybrid layer, inefficient infiltration / penetration of the primer components in demineralized collagen fibrils, level of the hydration of the substrates in the dentin, incomplete evaporation of the solvent from the dentin surface before the bonding of the adhesive monomers, incompatibility of the bonding agent with the respective resin compound, the composition of the acid component (pH, osmolarity , and thickening agent), polymerization shrinkage, physical characteristics of matter l Restoration (filling load, volumetric expansion and modulus of elasticity), inadequate adaptation of the margin of the restorative material, incompatibilities of source-photoinitiator and instrumentation polymerization and the effects of polishing and finishing should be effective since if they are deficient they produce gingival irritation and inflation subsequently producing bone crest loss, gingival recession or gingival hyperplasia15,16,21–23.
Unfortunately, all these approaches have not provided a satisfactory solution. Several researchers have suggested painting a resin of low viscosity on the resin and tooth interface to re-seal the margins of the restoration, particularly those of dentin. The concept of re-sealing of marginal fissures consists in applying a resin bonding agent without filler along the edges of the finished restorations. This compensates for the adverse effect of the polymerization contraction at the tooth-restoration interface and guarantees greater quality and durability of the marginal adaptation16.
Some authors have indicated that, despite the constant development of dentin binding adhesives and the application of hybrid glass ionomer materials and composite resins, the marginal seal of restorations still deserves considerable study24,25. Another study showed that the degree of contraction, stiffness of the materials and the resistant bond to the dental structure can predict the performance of material when microfiltration is analyzed26. The choice of technique, materials and placement are determining factors of microfiltration27,28. Surface sealers must be applied before finishing and polishing. This is especially recommended because the finish can block the micro spaces of debris and prevent the penetration of sealing agents into the composite once finished29. Any excess heat generated during finishing and polishing can cause the coating agent to collapse on the polymerized restoration and the reopening of the gap. On the other hand, the finishing procedures could lead to the reopening of the marginal lagoons due to the difference in the coefficient of thermal expansion between structures, it is very important to polish the material so that it is not over-contoured and there is no periodontal condition30.31. In the same way it has been recommended to place the rebonding agent after finishing the restoration, thus helping to improve periodontal health in a restoration so close to the periodontium32.
The discrepancies between the studies may be due to differences in the type of teeth or crowns, core materials, storage time, pH of the medium, fixing cement and evaluation methods2.
The main limitation of this study is its in vitro design, and the experimental conditions we use since it cannot be assumed to be totally equivalent to the conditions in vivo. Additional clinical studies should be designed to compare the performance of different types of basic materials used for class V restorations2.31–33.
Conclusions
Under the limitations of this study, it can be concluded that microfiltration of the ketac molar glass ionomer is greater due to its low fracture resistance, low modulus of elasticity, as indicated by the results of the studies.
Bibliografía
- ang S, Lee H, Jin S-H. A combined approach to non-carious cervical lesions associated with gingival recession. Restor Dent Endod. 2016;41(3):218.
- Perez CDR, Gonzalez MR, Prado NAS, de Miranda MSF, Macêdo M de A, Fernandes BMP. Restoration of noncarious cervical lesions: when, why, and how. Int J Dent. 2012;2012:687058.
- Memarpour M, Derafshi R, Razavi M. Comparison of microleakage from stainless steel crowns margins used with different restorative materials: An in vitro study. Dent Res J (Isfahan). 2016;13(1):7–12.
- Naik V-K, Jacob C-A, Nainar D-A. Assessment of non-carious root surface defects in areas of gingival recession: A descriptive study. J Clin Exp Dent. 2016;8(4):e397–402.
- Carlo B, Barabanti N, Piccinelli G, Faus-Matoses V, Cerutti A. Microbiological characterization and effect of resin composites in cervical lesions. J Clin Exp Dent. 2017;9(1):e40–5.
- Lanata EJ. Operatoria Dental. 1st ed. Buenos Aires; 2003. 322 p.
- Luong E, Shayegan A. Assessment of microleakage of class V restored by resin composite and resin-modified glass ionomer and pit and fissure resin-based sealants following Er:YAG laser conditioning and acid etching: in vitro study. Clin Cosmet Investig Dent. 2018;10:83–92.
- Sadeghi M, Davari A, Lynch CD. The effect of re-bonding using surface sealant or adhesive system on microleakage of class V resin composite restorations. Dent Res J (Isfahan). 2013;10(5):596–601.
- Nematollahi H, Bagherian A, Ghazvini K, Esmaily H, Mehr MA. Microbial microleakage assessment of class V cavities restored with different materials and techniques: A laboratory study. Dent Res J (Isfahan). 2017;14(5):344–50.
- Lee JJ, Nettey-Marbell A, Cook A, Pimenta LAF, Leonard R, Ritter A V. Using Extracted Teeth for Research: The Effect of Storage Medium and Sterilization on Dentin Bond Strengths. J Am Dent Assoc. 2007;138(12):1599–603.
- Gupta J, Thomas MS, Radhakrishna M, Srikant N, Ginjupalli K. Effect of silver diamine fluoride-potassium iodide and 2% chlorhexidine gluconate cavity cleansers on the bond strength and microleakage of resin-modified glass ionomer cement. J Conserv Dent. 2019;22(2):201–6.
- Selvaraj K, Sampath V, Sujatha V, Mahalaxmi S. Evaluation of microshear bond strength and nanoleakage of etch-and-rinse and self-etch adhesives to dentin pretreated with silver diamine fluoride/potassium iodide: An in vitro study. Indian J Dent Res. 2016;27(4):421.
- Hernández M. Aspectos prácticos de la adhesión a dentina. Av Odontoestomatol. 2004;6(1):19–32.
- Jordehi AY, Shahabi MS, Akbari A. Comparison of self-adhering flowable composite microleakage with several types of bonding agent in class V cavity restoration. Dent Res J (Isfahan). 2019;16(4):257–63.
- Sooraparaju SG, Kanumuru PK, Nujella SK, Konda KR, Reddy KBK, Penigalapati S. A Comparative Evaluation of Microleakage in Class V Composite Restorations. Int J Dent. 2014;2014:1–4.
- Gupta A, Tavane P, Gupta PK, Tejolatha B, Lakhani AA, Tiwari R, et al. Evaluation of Microleakage with Total Etch, Self Etch and Universal Adhesive Systems in Class V Restorations: An In vitro Study. J Clin Diagn Res. 2017;11(4):ZC53–6.
- Bollu IP, Hari A, Thumu J, Velagula LD, Bolla N, Varri S, et al. Comparative Evaluation of Microleakage Between Nano-Ionomer, Giomer and Resin Modified Glass Ionomer Cement in Class V Cavities-CLSM Study. J Clin Diagnostic Res JCDR. 2016;10(5):ZC66.
- Kumar U, Dharmani CKK, Singh S, Logani A, Shah N. Effect of Air Abrasion Preconditioning on Microleakage in Class V Restorations Under Cyclic Loading: An In-vitro Study. J Clin Diagn Res. 2014 May;8(5):ZC29-32.
- Sharafeddin F, Yousefi H, Modiri S, Tondari A, Safaee Jahromi S. Microleakage of Posterior Composite Restorations with Fiber Inserts Using two Adhesives after Aging. J Dent Shiraz Univ Med Sci. 2013;14(143):90–5.
- Bortolotto T, Betancourt F, Krejci I. Marginal integrity of resin composite restorations restored with PPD initiatorcontaining resin composite cured by QTH, monowave and polywave LED units. Dent Mater J. 2016;35(6):869–75.
- Yoshimine N, Shimadab Y, Tagami J, Sadr A. Interfacial Adaptation of Composite Restorations Before and After Light Curing: Effects of Adhesive and Filling Technique. J Adhes Dent. 2015;17(4):329–36.
- Al-Agha EI, Alagha MI. Nanoleakage of Class V Resin Restorations Using Two Nanofilled Adhesive Systems. J Int Oral Heal. 2015;7(7):6–11.
- Mamaladze M, Khutsishvili L, Zarkua E. Distribution of carious and non-carious cervical lesions and gingival recession at age related aspects. Georgian medical news. Georgian Med News. 2016;7–8(256–257):18–22.
- Casselli DSM, Faria-E-Silva AL, Casselli H, Martins LRM. Marginal adaptation of class V composite restorations submitted to thermal and mechanical cycling. J Appl Oral Sci. 2013 Feb;21(1):68–73.
- Doozandeh M, Shafiei F, Alavi M. Microleakage of Three Types of Glass Ionomer Cement Restorations: Effect of CPP-ACP Paste Tooth Pretreatment. J Dent (Shiraz, Iran). 2015;16(3):182–8.
- Pereira J-R, Júnior L-C, Só M-V-R, Júnior N-F. Effect of thermocycling and varying polymerization techniques on the restorative interface of class V cavities restored with different composite resin systems. J Clin Exp Dent. 2017;9(3):e405–9.
- Mozaffari HR, Ehteshami A, Zallaghi F, Chiniforush N, Moradi Z. Microleakage in Class V Composite Restorations after Desensitizing Surface Treatment with Er:YAG and CO2 Lasers. Laser Ther. 2016;25(4):259–66.
- Patnana AK, Vanga VNR, Chandrabhatla SK. Evaluating the Marginal Integrity of Bulk Fill Fibre Reinforced Composites in Bio-mimetically Restored Tooth. J Clin Diagn Res. 2017 Jun;11(6):ZC24–7.
- Gopinath V. Comparative evaluation of microleakage between bulk esthetic materials versus resin-modified glass ionomer to restore class II cavities in primary molars. J Indian Soc Pedod Prev Dent. 2017;35(3):238.
- Alizadeh Oskoee P, Pournaghi Azar F, Jafari Navimipour E, Ebrahimi Chaharom ME, Naser Alavi F, Salari A. The effect of repeated preheating of dimethacrylate and silorane-based composite resins on marginal gap of class V restorations. J Dent Res Dent Clin Dent Prospects. 2017;11(1):36–42.
- Altunsoy M, Tanrıver M, Türkan U, Uslu ME, Silici S. In Vitro Evaluation of Microleakage and Microhardness of Ethanolic Extracts of Propolis in Different Proportions Added to Glass Ionomer Cement. J Clin Pediatr Dent. 2016;40(2):136–40.
- Garcia-Godoy F, Malone WF. Microleakage of posterior composite restorations after rebonding. Compendium. 1987;8(8):606–9.
- Han S-H, Sadr A, Tagami J, Park S-H. Non-destructive evaluation of an internal adaptation of resin composite restoration with swept-source optical coherence tomography and micro-CT. Dent Mater. 2016 Jan;32(1):e1–7.
 |
Eliana Carolina Morillo Cárdenas; https://orcid.org/0000-0001-5301-288X |
| Jennyfer Marybel García Cárdenas; https://orcid.org/0000-0001-9035-7668 |
| María Elena Flores Araque; https://orcid.org/0000-0002-8502-4102 |
| César Paz-y-Miño; https://orcid.org/0000-0002-6693-7344 |
| Paola E. Leone; https://orcid.org/0000-0003-3351-2275 |

Reconocimiento-NoComercial-CompartirIgual
CC BY-NC-SA
Esta licencia permite a otros entremezclar, ajustar y construir a partir de su obra con fines no comerciales, siempre y cuando le reconozcan la autorÍa y sus nuevas creaciones estÉn bajo una licencia con los mismos tÉrminos.