Dental treatment in patients with heart disease and use of warfarin.
DOI:
https://doi.org/10.29166/odontologia.vol24.n2.2022-e3941Keywords:
Warfarin, Heparin, Bleeding, Bridging Therapy, Thromboembolism, pre heart attackAbstract
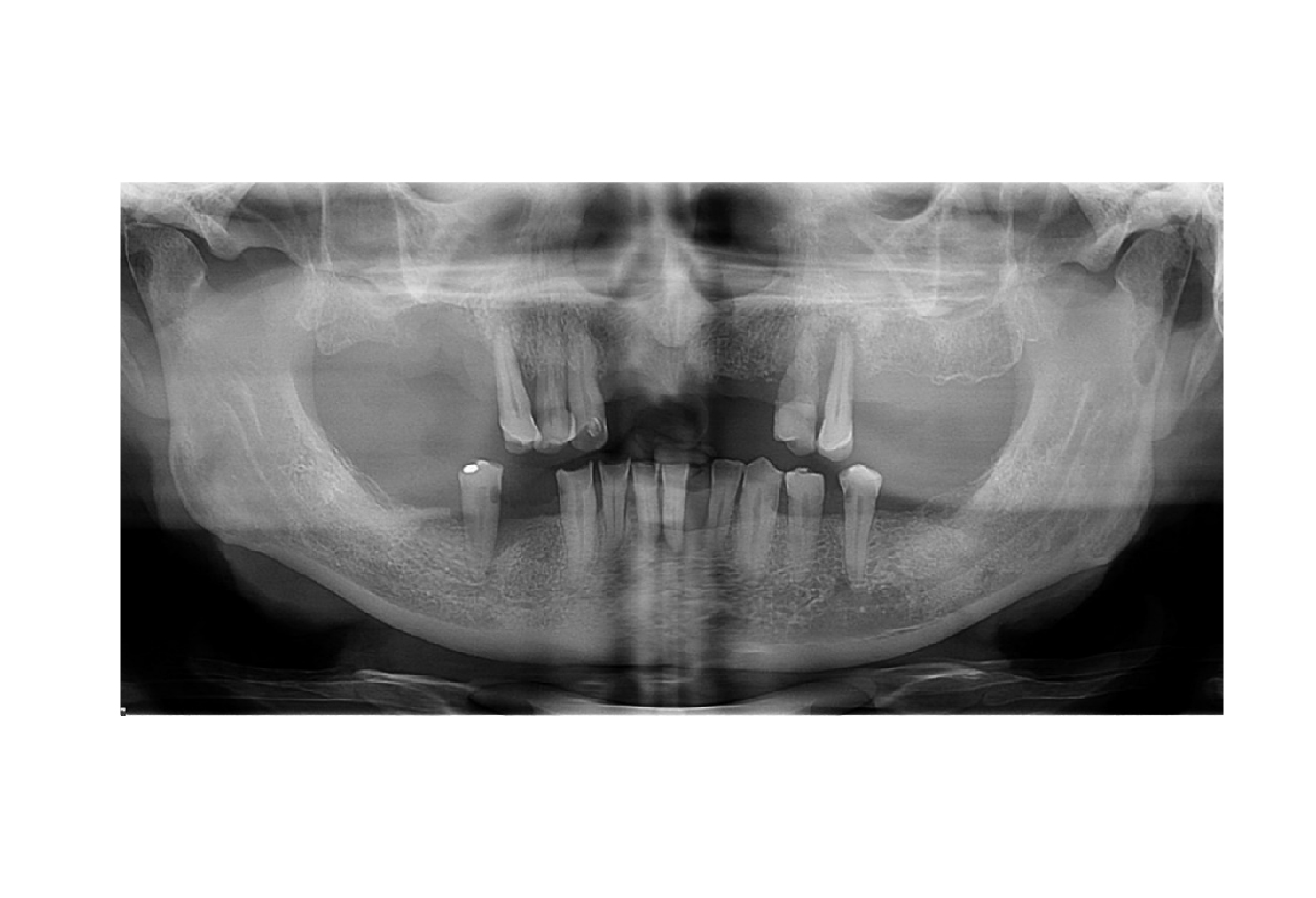
Dental treatment in people with cardiac disorders such as pre-infarction or valve surgeries, who use anticoagulants such as warfarin and have poor oral hygiene should be planned from the beginning between the dentist, specialists and even doctors (cardiologists, hematologists, surgeons, etc.). Substituting warfarin for low molecular weight heparin (LMWH) as bridging therapy in the case of multiple extractions is the best alternative to avoid complications of heavy bleeding and/or thromboembolism. In this case the best choice was the use of Enoxaparin. The use of antibiotics also contributes to the success of the treatment, avoiding infections after the surgical procedure and even more so if the patient has pre-existing conditions. Precaution with appropriate therapeutic protocols the integrity of the patient before, during and after performing multiple extractions; thus avoiding abundant bleeding, possible postoperative infection and/or systemic decompensation. A 67-year-old male patient with 2 pre-infarctions and heart valve surgery with poor oral hygiene requires: prophylaxis, removal of dental calculus and multiple extractions to subsequently execute total upper acrylic dental prostheses and lower cobalt chrome prostheses to improve aesthetics and chewing function. Two weeks after the multiple extractions, the prosthetic area is in excellent condition and dental prostheses with excellent adaptability, stability, functionality and good aesthetics could be made. Applying bridging therapy with enoxaparin was the best alternative to avoid profuse bleeding and/or formation of thromboembolism that could lead to systemic complications for the patient.Downloads
References
James W, Donald A, Craig S, Nelson I. Tratamiento odontológico del paciente bajo tratamiento médico. 5.a ed. Madrid-España. Editorial Harcourt. 1998.
Díaz M, Rosales A, Neri R, Espinosa I. Reversión de la anticoagulación en el perioperatorio. Revista mexicana de Anestesiología [Internet] 2014 octubre-diciembre;37(2):414-422. https://www.medigraphic.com/cgi-bin/new/resumen.cgi?idarticulo=54279
Mora J, Manejo de nuevos anticoagulantes orales en cirugía oral. Revisión de literatura. Universidad de los Andes Santiago, Chile. Odontología [Internet] 2020 julio;22(2):72-91. https://revistadigital.uce.edu.ec/index.php/odontologia/article/view/2219/2442
Martínez F. Protocolo de actuación clínica ante pacientes anticoagulados farmacológicamente. Sociedad Española de Odontoestomatología para pacientes con necesidades especiales [Internet]. https://www.seoene.es/protocolo-de-actuacion-clinica-ante-pacientes-anticoagulados-farmacologicamente/
Ripollés J, Gómez R, Muñoz M, Bascones A. Actualización en los protocolos de extracción dental en pacientes anticoagulados. Avances Odonto estomatol [Internet] 2012;2(6):311-320. https://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0213-12852012000600006
Yurgaky J, Rodríguez F. Warfarina: uso contemporáneo. Revista Med [Internet] 2009 enero-junio;17(1):107-115. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0121-52562009000100015
Gallego C, Ferreira FJ, Guerrero N, Olmos L. Terapia puente con anticoagulantes de administración parenteral de acción corta en pacientes anticoagulados con antagonistas de vitamina K sometidos a un procedimiento invasivo programado. Pharm Care Esp [Internet] 2017;19(3):153-157. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahukewiotqf8_sx2ahxtstabhztnat8qfnoecauqaw&url=https%3a%2f%2fwww.pharmcareesp.com%2findex.php%2fpharmacare%2farticle%2fdownload%2f403%2f297%2f890&usg=aovvaw0p3hw3fuvqnqvjtz9v9ndl
Cuevas M, Cuevas B, García C. La utilidad de la terapia puente en la anticoagulación oral. Revista Electrónica de Biomedicina [Internet] 2018;1:49-57 https://biomed.uninet.edu/2018/n1/mvcuevas.html
Pérez M, García C, Duro E, Díaz P. Revisión del manejo perioperatorio de anticoagulantes y antiagregantes. Anestesiar. Anestesia general [Internet] 2022 febrero. https://anestesiar.org/2022/revision-del-manejo-perioperatorio-de-anticoagulantes-y-antiagregantes/
Nazar C, Cárdenas A, Coloma R, Contreras J, Molina I, Miranda P, Fuentes R. Manejo perioperatorio de pacientes con tratamiento anticoagulante crónico. Revista chilena de cirugía [Internet]. 2017;190:1-8. https://www.elsevier.es/es-revista-revista-chilena-cirugia-266-avance-resumen-manejo-perioperatorio-pacientes-con-tratamiento-S0379389317301084
López R. Warfarina y sus interacciones con medicamentos de atención primaria. Revista médica de Costa Rica y Latinoamérica [Internet]. 2014;612:745-752 https://www.medigraphic.com/cgibin/new/resumen.cgi?idarticulo=56825
Idrobo P, Gutiérrez K, Castillo G, Ordóñez A. Antibióticos indicados en Odontología. Revista oactiva uc Cuenca [Internet] 2019; diciembre;4:63-68. https://oactiva.ucacue.edu.ec/index.php/oactiva/article/view/409
Moreno A, Gómez J. Terapia antibiótica en odontología de práctica general. Revista adm [Internet]. 2012 julio-agosto;69(4):168-175. https://www.medigraphic.com/pdfs/adm/od-2012/od124e.pdf
Méndez R, Méndez A, Torres J. Antibioticoterapia en odontología: ¿uso racional o indiscriminado? Salud en Tabasco [Internet] 2013 mayo-agosto;19(2):62-65. https://www.redalyc.org/articulo.oa?id=48729883005
Published
How to Cite
Issue
Section
License

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.